Research
Findings #8: Health Insurance Status of the Civilian Noninstitutionalized
Population, 1997
Jessica P. Vistnes, Ph.D., and Samuel H. Zuvekas,
Ph.D., Agency for Health Care Policy and Research.
Abstract This report from the 1997 Medical Expenditure Panel Survey (MEPS) provides preliminary estimates of the health insurance status of the civilian noninstitutionalized U.S. population during the first half of 1997, including the size and characteristics of the population with private health insurance, with public insurance, and without any health care coverage. During this period, 83.2 percent of all Americans were covered by private or public health insurance, leaving 16.8 percent of the population, some 44.6 million persons, uninsured. Among the non-elderly population, 81.1 percent of Americans had either private or public coverage and 18.9 percent of the population (44.2 million persons) lacked health care coverage. The probability that an individual would be uninsured during this period was especially high for young adults aged 19-24 and members of racial and ethnic minorities (especially Hispanic males). Public health insurance continues to play an important role in ensuring that children, black Americans, and Hispanic Americans obtain health care coverage.
^top
Introduction This report is the second in a series of yearly
reports on the health insurance status of the U.S. population.
The first report (Vistnes and Monheit, 1997) presented health insurance
estimates for the first half of 1996.
The health insurance status of the U.S. population,
especially the size and composition of the uninsured population,
has become an issue of perennial public policy concern for several
reasons.
First,
health insurance is viewed as essential to ensure that individuals
obtain timely access to medical care and protection against the
risk of expensive and unanticipated medical events. Compared to
people without health care coverage, insured individuals are more
likely to have a usual source of medical care, to spend less out
of pocket on health services, and to experience different treatment
patterns, quality, and continuity in their health care (Lefkowitz
and Monheit, 1991; U.S. Congress, Office of Technology Assessment,
1992).
Second, concern over
the population’s health
insurance status reflects a variety of equity and efficiency considerations.
These include the magnitude and appropriate mix of private and
public sector responsibility for financing health care, the impact
of health insurance on the efficient use of health care, and the
manner in which health insurance affects the distribution of health
care among the general population and across groups of specific
policy interest.
Third, timely and
reliable estimates of the population’s
health insurance status are essential to evaluate the costs and
expected impact of public policy interventions to expand coverage
or to alter the manner in which private and public insurance is
financed. Identification of how individual and household demographic
characteristics, health status, and economic circumstances are
associated with the population’s health insurance status is
of critical importance in developing efficient and targeted policy
interventions. This is especially relevant given the current emphasis
on incremental health care reform that is focused on particular
health care markets and population groups.
Finally, comparisons
of the characteristics of insured and uninsured populations over
time provide information
on whether greater equity has been achieved in the ability of specific
population groups to obtain health insurance or whether serious
gaps remain. In this regard, estimates of the population’s
health insurance status from the Medical Expenditure Panel Survey
(MEPS), which is conducted annually, provide critical data for
evaluating the health insurance implications of recent legislative
initiatives: the 1996 Health Insurance Portability and Accountability
Act (HIPAA), Public Law 104-191; welfare reform under the 1996
Personal Responsibility and Work Opportunity Reconciliation Act,
Public Law 104-193; and the 1997 State Children’s Health Insurance
Program (CHIP). A primary goal of HIPAA is to reduce the impact
of preexisting health conditions on the continuity of health insurance
during employment transitions. Under welfare reform, mandated work
requirements and time limitations governing the receipt of public
assistance may have consequences for a recipient’s health
insurance status. The goal of the CHIP program is to provide health
insurance coverage to low-income children who are not eligible
for Medicaid.
This report presents
preliminary estimates of the number and characteristics of people
with private and public
health insurance at any time during the first half of 1997, on
average. Particular emphasis is directed toward estimating the
size of the population that was uninsured throughout the first
half of 1997 and identifying groups especially at risk of lacking
health insurance.
^top
Overview
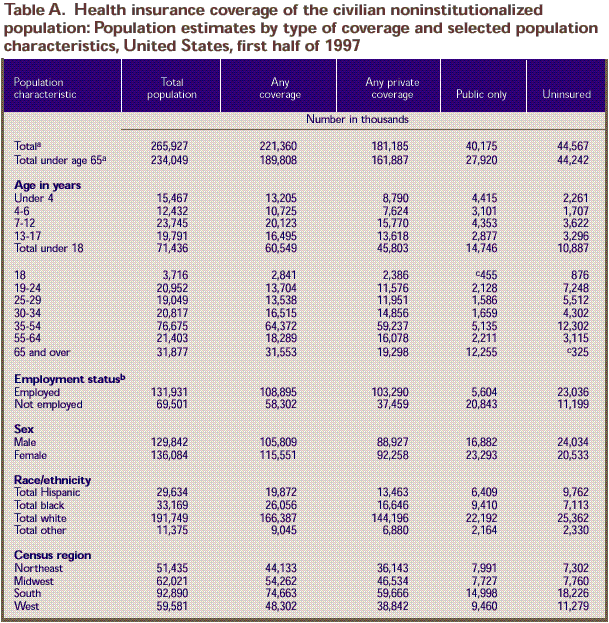
During the first half of
1997, on average, 83.2 percent of all Americans in the civilian
noninstitutionalized population
had some type of private or public health insurance coverage (Table
1). Roughly 68 percent of Americans obtained health insurance
from private sources.Another 15.1 percent obtained public sources
of coverage, primarily from the Medicare and Medicaid programs.
The remaining 16.8 percent of Americans, 44.6 million people, were
without health insurance throughout the first half of 1997. Among
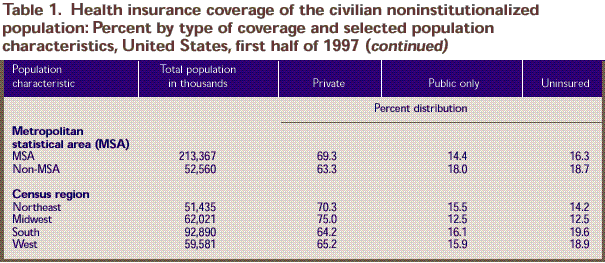
the non-elderly population, 69.2 percent were covered by private
insurance and 11.9 percent by public insurance. Almost a fifth
of the non-elderly population (18.9 percent), an estimated 44.2
million people, were uninsured. Table 2 gives
more detailed information on the health insurance status of the
non-elderly population. Overall, these health insurance estimates
do not differ significantly from the 1996 MEPS figures reported
in Vistnes and Monheit, 1997.
The data in Tables 1-3 provide
estimates of the population’s health insurance status according
to selected demographic characteristics, perceived health status,
employment status, and residential location. Table
4 provides estimates of the distribution of the uninsured population
by selected characteristics. Table A in the Technical Appendix
provides estimates of the number of people by health insurance
status. Some of the key findings and relationships revealed by
these data are discussed below.
Age MEPS data reveal that, in general, children are
more likely than non-elderly adults to have health insurance coverage.
The main findings among age groups are described below.
Children There has been considerable
interest in the health insurance status of children. This interest
stems from the role
health care coverage plays in ensuring that children obtain the
medical care appropriate to their specific stage of development.
To help ensure such coverage, Congress passed the State Children’s
Health Insurance Program in 1997, allocating approximately $24
billion over 5 years to provide health insurance coverage to low-income
children who are not eligible for Medicaid. The CHIP program follows
on Medicaid expansions beginning in the late 1980s that focused
attention on the role of the public and private sectors in financing
health care for low-income children.MEPS data indicate that public health insurance
covered a substantial proportion of children in the first half
of 1997: Nearly 30 percent of children under age 4, one in four
children ages 4-6, and close to one in five children ages 7-12
had public coverage, primarily through Medicaid. As a result, children
under age 18 were less likely to be uninsured than were non-elderly
adults in general. Despite this finding, nearly 11 million children
lacked health care coverage.
Adults Young adults ages 19-24 were the age group most
likely to lack health insurance. Over a third of young adults (34.6
percent) were uninsured, twice the rate at which all Americans
lacked coverage. Young adults ages 19-24 also had the lowest rate
of private health insurance coverage among the non-elderly adult
population.On the other hand, 6 out
of 10 elderly Americans (60.5 percent) were covered by private
health insurance. Nearly
4 out of 10 elderly Americans (38.4 percent) held only public coverage
(Medicare alone or in conjunction with Medicaid).
Employment Status
Since most private health
insurance in the United States is provided through the workplace,
employment status is
an important indicator of access to private health insurance.
MEPS data reveal the following for the non-elderly population (Table
2):
- Over three-quarters
(78.7 percent) of workers were covered by private health insurance,
compared to half (50.3
percent) of individuals who were not employed.
- People who were not employed were more likely
than those who were employed to be covered by public insurance
(23.9 and 3.2 percent, respectively). Workers
were less likely than people who were not employed to be uninsured
(18.0 and 25.9 percent,
respectively).
Race/Ethnicity
MEPS data indicate that significant disparities
exist in the rate at which racial and ethnic minorities are covered
by private and public health insurance compared to white Americans (Table
1). For example:
- Less than half of all Hispanic Americans (45.4
percent) and half of black Americans (50.2 percent) were covered
by private health insurance, compared to three-quarters of whites
(75.2 percent). A third of Hispanics (32.9 percent) and over
a fifth of blacks (21.4 percent) were uninsured. In contrast,
13.2 percent of white Americans were uninsured.
- Among all racial/ethnic groups, Hispanic males
were the most likely to be uninsured; 36.9 percent lacked coverage.
Hispanic and black Americans were more likely
than white Americans to be covered by public health insurance (21.6
percent and 28.4 percent, respectively, compared to 11.6 percent).
Marital Status
Married individuals were more likely than others
to have private health insurance (Table 1).
Of those who were not married at the time of the survey:
- Widowed people were the least likely to be
uninsured (6.5 percent) because of their higher rate of coverage
from public programs (39.4 percent).
- More than one-quarter of Americans who never
married were uninsured (27.4 percent).
- Almost a third of Americans who were separated
were uninsured (31.9 percent).
- More than a fifth of all divorced persons
(21.2 percent) were uninsured.
Residential Location
The type of health care coverage obtained by
Americans and the likelihood of being uninsured also varied by
region and whether they lived in a metropolitan statistical area
(MSA). MEPS data show that: People living
in the South and West were less likely than residents of other
regions to have private
health insurance (64.2 percent and 65.2 percent in the South
and West, respectively, compared to 70.3 percent and 75.0
percent of residents in the Northeast and Midwest). Nearly one
out of five persons in the South and West were uninsured (19.6
percent and 18.9 percent, respectively) compared to14.2
and 12.5 percent in the Northeast and Midwest, respectively.
- People living outside
MSAs were less likely than those living within MSAs to be covered
by private
health insurance (63.3 percent vs. 69.3 percent). They also were
more likely to be uninsured (18.7 percent vs. 16.3 percent).
Health Status
There is considerable
public policy interest in determining whether people with health
problems are able to
obtain health insurance and, if so, the source of such coverage.
MEPS respondents were asked to rate their health and family members’ health
as excellent, very good,good, fair, or poor. The data in Table
3 reveal the relationships described below between health status
and insurance coverage.
Non-Elderly Persons
More than one in five non-elderly Americans in
good health (22.9 percent), fair health (23.4 percent), or poor
health (21.2 percent) were uninsured throughout the first half
of 1997. Among the non-elderly:
- People in fair or poor health were less likely
than those in better health to have private health insurance.
Only 39.3 percent of those in poor health and 54.2 percent of
those in fair health had any private coverage.
- Public insurance helped to reduce the health-related
disparities in private coverage. Over 20 percent of people in
fair health and almost 40 percent of people in poor health had
public coverage.
Elderly Persons
Elderly Americans in fair or poor health were
less likely to have private coverage than those in better health.
As a result, those in fair or
poor health were more likely
to be covered by insurance from public sources only (43.5 and 55.7
percent,
respectively) than other elderly Americans. Medicare, either
alone or with Medicaid, was the main public source of coverage.
^top
Characteristics
of Uninsured Americans
Previous sections of this report have described
the health insurance status of Americans by focusing on demographic,
health status, and geographic characteristics associated with the
likelihood that particular groups obtained private or public health
insurance or were more at risk of being uninsured. To put this
discussion in perspective, data displayed in Table 4 characterize
the uninsured population by considering the representation of specific
groups in the general population of non-elderly Americans relative
to their representation among the uninsured population. In this
way, one can assess whether certain population groups are disproportionately
represented among the uninsured. Such information can be useful
in formulating targeted policy interventions on behalf of people
without health insurance.
Age
Young adults ages 19-24 composed 9.0 percent
of the non-elderly population but 16.4 percent of the uninsured
population. Among all age groups, young adults had the greatest
risk of being uninsured.
Race/Ethnicity
Racial and ethnic minorities were more at risk
of lacking health insurance than white Americans were. As a result,
minority representation among the uninsured exceeded their representation
among the general population. For example:
- Although Hispanics represented only 12.0 percent
of the non-elderly U.S. population, they accounted for 22.0 percent
of the uninsured population.
- Hispanic males represented only 6.2 percent
of all non-elderly Americans but were the racial/ethnic group
most likely to be uninsured, comprising 12.6 percent of the uninsured
population.
- Although 7 out of 10 non-elderly Americans
were white, whites accounted for less than 6 out of 10 uninsured
persons.
- When the uninsured are categorized by race/ethnicity
and sex, white males represent the largest proportion of the
uninsured population.
Other Factors
People with specific residential locations and
marital status were also disproportionately represented among the
uninsured:
- People living in the South represented about
a third (34.8 percent) of all non-elderly Americans but 40.9
percent of all uninsured Americans.
- People who never
married accounted for over a fifth of the non-elderly population
but over a third of the
uninsured population.
Finally, more than 1 out of 10 uninsured people
(10.5 percent of the uninsured population) were in fair or poor
health. These individuals are of particular policy concern because
of the importance of health insurance in assuring timely access
to needed health care services.
^top
Conclusions
Preliminary estimates from the 1997 MEPS reveal
that, during the first half of 1997, 68.1 percent of Americans
obtained health insurance from private sources, 15.1 percent obtained
coverage through public programs, and 16.8 percent of the population
(44.6 million people) lacked any health care coverage. Among the
non-elderly population, nearly one person in five was uninsured.
The tabulations presented in this report indicate
that the health insurance status of the U.S. population
is strongly associated with specific demographic characteristics,
health status, and employment status. Important disparities in
health care coverage exist for particular groups. Among the groups
especially at risk of lacking health care coverage are young adults
ages 19-24 and members of racial and ethnic minorities (especially
Hispanic males). Public health insurance continues to play an important
role in insuring children, black Americans, and Hispanic Americans.
Disparities in rates of insurance coverage also exist by health
status, with non-elderly people in good or fair health more likely
than people in better health to be uninsured.
^top
Tables
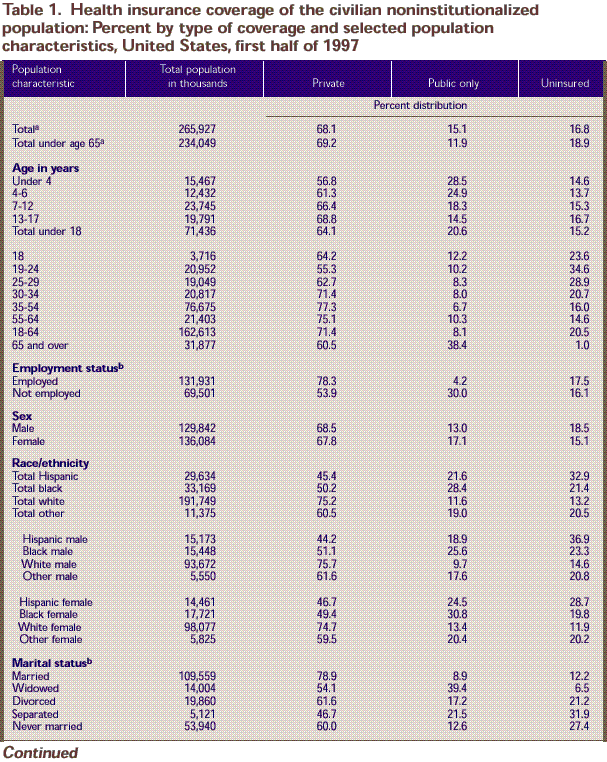
a Includes persons with
unknown employment status and marital status.
b For individuals age 16
and over.
Note: Percents
may not add to 100 because of rounding. Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
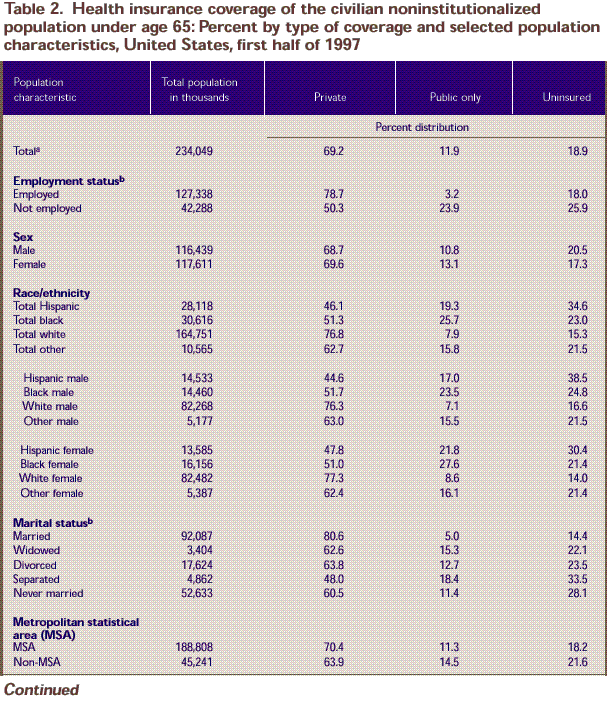
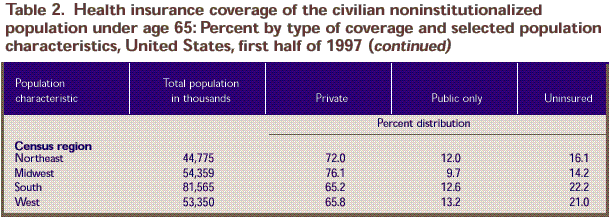
a Includes persons with
unknown employment status and marital status.
b For individuals age 16
and over.
Note: Percents
may not add to 100 because of rounding.
Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
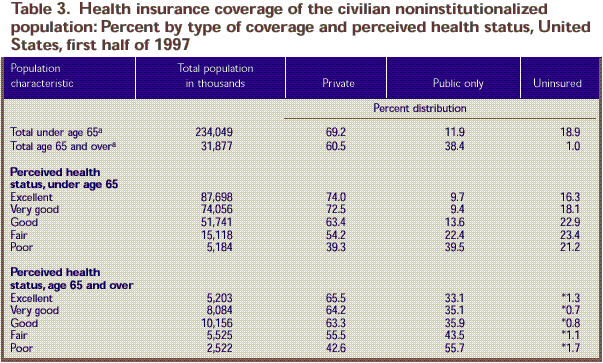
a Includes persons with
unknown perceived health status.
* Relative standard error
is greater than or equal to 30 percent.
Note: Percents
may not add to 100 because of rounding.
Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
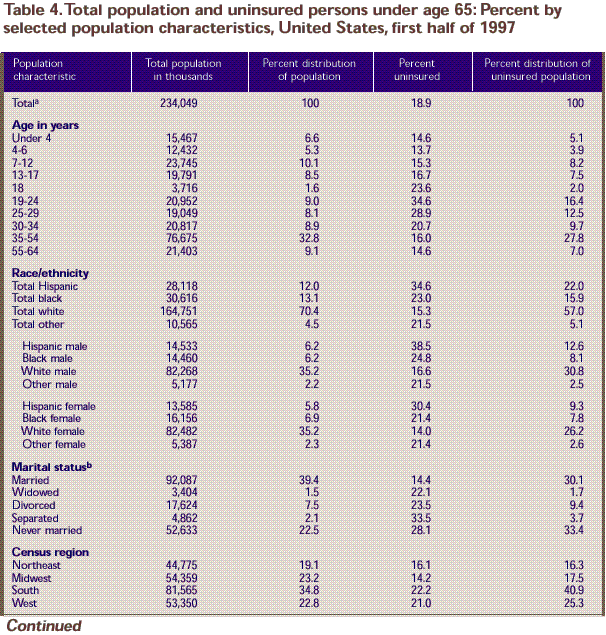
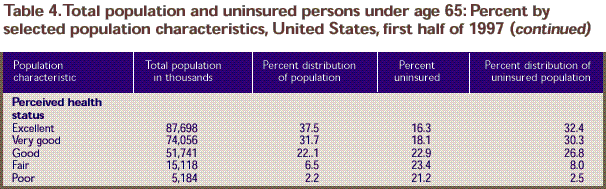
a Includes persons with
unknown marital status and perceived health status.
b For individuals age 16
and over. Excludes unknown marital status. As a result, percents
do not sum to 100.
Note: Percent
distributions may not add to 100 because of rounding.
Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
References
Cohen JW, Monheit AC, Beauregard KM, et al. The
Medical Expenditure Panel Survey: a national health information
resource. Inquiry 1996;33:373-89.
Cohen S. Sample design of the 1996 Medical Expenditure
Panel Survey Household Component. Rockville (MD): Agency for Health
Care Policy and Research; 1997. MEPS Methodology Report No. 2.
AHCPR Pub. No. 97-0027.
Lefkowitz D, Monheit AC. Health insurance, use
of health services, and health care expenditures. Rockville (MD):
Agency for Health Care Policy and Research; 1991. National Medical
Expenditure Survey Research Findings 14. AHCPR Pub. No. 92-0017.
U.S. Congress, Office of Technology Assessment.
Does health insurance make a difference? Background paper. Washington:
U.S. Government Printing Office; 1992. Report No. OTA-BP-H-99.
Vistnes, JP, Monheit, AC. Health insurance status
of the civilian noninstitutionalized population: 1996. Rockville
(MD): Agency for Health Care Policy and Research; 1997. MEPS Research
Findings No. 1. AHCPR Pub. No. 97-0030.
^top
Technical Appendix
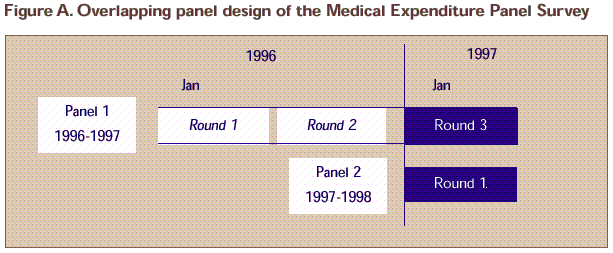
The data in this report were obtained in the
third round of interviews for the Household Component (HC) of the
1996 Medical Expenditure Panel Survey (MEPS) and the first round
of interviews from the 1997 MEPS HC. MEPS is cosponsored by the
Agency for Health Care Policy and Research (AHCPR) and the National
Center for Health Statistics (NCHS). The MEPS HC is a nationally
representative survey of the U.S. civilian noninstitutionalized
population that collects medical expenditure data at both the person
and household levels. The focus of the MEPS HC is to collect detailed
data on demographic characteristics, health conditions, health
status, use of medical care services, charges and payments, access
to care, satisfaction with care, health insurance coverage, income,
and employment. In other components of MEPS, data are collected
on the use, charges, and payments reported by providers; residents
of licensed or certified nursing homes; and the supply side of
the health insurance market.
The sample for the MEPS HC was selected from
respondents to the National Health Interview Survey (NHIS), which
was conducted by NCHS. NHIS provides a nationally representative
sample of the U.S. civilian noninstitutionalized population and
reflects an oversampling of Hispanics and blacks. The MEPS HC collects
data through an overlapping panel design. In this design, data
are collected through a precontact interview that is followed by
a series of five rounds of interviews over 21¼2 years.
Two calendar years of medical expenditure and utilization data
are collected from each household and captured using computer-assisted
personal interviewing (CAPI). This series of data collection rounds
is launched again each subsequent year on a new sample of households
to provide overlapping panels of survey data which, when combined
with other ongoing panels, will provide continuous and current
estimates of health care expenditures. The reference period for
Round 3 of the 1996 MEPS HC (Panel 1) was from the Round 2 interview
date to the Round 3 interview date. The reference period for Round
1 of the 1997 MEPS HC (Panel 2) was from January 1, 1997, to the
date of the Round 1 interview. Interviews for Panel 1 (Round 3)
and Panel 2 (Round 1) were conducted from March to July 1997.
Derivation
of Insurance Status Information
The household respondent
was asked if during the interview period anyone in the family
was covered by any of
the sources of public and private health insurance coverage discussed
in the following paragraphs. For respondents in their third MEPS
interview (Panel 1), previously reported insurance was reviewed
to determine whether it was still in effect and when changes in
insurance status had occurred. Although Panel 1 survey respondents
were asked about their insurance information for part of 1996 as
well as 1997, the insurance information in this report refers to
coverage only in 1997. Medicare and CHAMPUS/CHAMPVA coverage were
measured at the time of the interview. (CHAMPUS and CHAMPVA are
the Civilian Health and Medical Programs for the Uniformed Services
and Veterans’ Affairs.) All other sources of insurance were
measured for any time between January 1997 and the interview. Persons
counted as uninsured were uninsured throughout this time period.
Public Coverage
For this report, individuals were considered
to have public coverage only if they met both of the following
criteria:
- They were not covered by private insurance.
- They were covered by one of the public programs
discussed below.
Medicare
Medicare is a federally financed health insurance
plan for the elderly, persons receiving Social Security disability
payments, and most persons with end-stage renal disease. Medicare
Part A, which provides hospital insurance, is automatically given
to those who are eligible for Social Security. Medicare Part B
provides supplementary medical insurance that pays for medical
expenses and can be purchased for a monthly premium.
CHAMPUS/CHAMPVA
CHAMPUS covers retired members of the Uniformed
Services and the spouses and children of active-duty, retired,
and deceased members. Spouses and children of veterans who died
from a service-connected disability, or who are permanently disabled
and are not eligible for CHAMPUS or Medicare, are covered by CHAMPVA.
In this report, CHAMPUS or CHAMPVA coverage is considered to be
public coverage. When persons covered by CHAMPUS/CHAMPVA reach
age 65, their coverage generally ends and enrollees are eligible
for Medicare.
Medicaid
Medicaid is a means-tested government program
jointly financed by Federal and State funds that provides health
care to those who are eligible. Program eligibility criteria vary
significantly by State, but the program is designed to provide
health coverage to families and individuals who are unable to afford
necessary medical care.
Other Public Hospital/Physician Coverage
Respondents who did not report Medicaid coverage
were asked if they were covered by any other public hospital/physician
coverage. These questions were asked in an attempt to identify
Medicaid recipients who might not have recognized their coverage
as Medicaid. In this report, all coverage reported in this manner
is considered public coverage.
Private Health Insurance
Private health insurance was defined for this
report as insurance that provides coverage for hospital and physician
care (including Medigap coverage). Insurance that provides coverage
for a single service only, such as dental or vision coverage, was
not counted. Private health insurance could have been obtained
through an employer, union, self-employed business, directly from
an insurance company or a health maintenance organization (HMO),
through a group or association, or from someone outside the household.
Uninsured
The uninsured were defined as persons not covered
by Medicare, CHAMPUS/CHAMPVA, Medicaid, other public hospital/physician
programs, or private hospital/physician insurance (including Medigap
coverage) during the period from January 1997 through the time
of the interview. Individuals covered only by noncomprehensive
State-specific programs (e.g., Maryland Kidney Disease Program)
or private single-service plans (e.g., coverage for dental or vision
care only, coverage for accidents or specific diseases) were not
considered to be insured.
Health Insurance
Edits
For the Round 1 (Panel 2) sample, minimal editing
was performed on sources of public coverage and no edits were performed
on the private coverage variables. For Round 3 (Panel 1), most
of the insurance variables were logically edited to address issues
that arose during Rounds 2 and 3 when reviewing insurance reported
in earlier rounds. The health insurance data were edited as described
below.
Medicare
Medicare coverage was edited for persons age
65 and over but not for persons under age 65. Persons age 65 and
over were assigned Medicare coverage if they met one of the following
criteria:
- They answered “yes” to
a follow-up question on whether they had received Social Security
benefits.
- They were covered by Medicaid, other public
hospital/physician coverage, or Medigap coverage.
- Their spouse was age 65 or over and covered
by Medicare.
- They were covered by CHAMPUS/CHAMPVA.
Medicaid
A small number of cases reporting Aid to Families
with Dependent Children (AFDC) or Supplemental Security Income
(SSI) coverage (questions included in the MEPS health insurance
section for editing purposes) were assigned Medicaid coverage.
Since this report does not distinguish among sources of public
insurance, no further edits were performed using the other public
hospital/physician coverage variables. Other public hospital/physician
coverage was included, however, when considering whether an individual
was covered only by public insurance.
CHAMPUS/CHAMPVA
Respondents age 65 and over who reported CHAMPUS/CHAMPVA
coverage were instead classified as covered by Medicare.
Private Health Insurance
Private insurance coverage was unedited and unimputed
for Round 1 (Panel 2). For Round 3 (Panel 1), most of the insurance
variables were logically edited to address issues that arose during
Rounds 2 and 3 when reviewing insurance reported in earlier rounds.
One edit to the private insurance variables corrected for a problem
concerning covered benefits when respondents reported a change
in any of their health insurance plan names. Additional edits addressed
issues of missing data on the time period of coverage.
Individuals were considered to be covered by
private insurance if the insurance provided coverage for hospital/physician
care. Medigap plans were included. Individuals covered by single-service
plans only (e.g., dental, vision, or drug plans) were not considered
to be privately insured. Sources of insurance with missing information
regarding the type of coverage were assumed to contain hospital/physician
coverage.
It should be noted that these data were generally
reported by a single household respondent, who may not have been
the most knowledgeable source for other family members. The employers
and insurance companies of household respondents are being contacted
in a follow-up survey as part of the MEPS data collection effort
designed to verify and supplement the information provided by the
household respondents.
Population
Characteristics
Place of Residence
Individuals were identified
as residing either inside or outside a metropolitan statistical
area (MSA) as designated
by the U.S. Office of Management and Budget (OMB), which applied
1990 standards using population counts from the 1990 U.S. census.
An MSA is a large population nucleus combined with adjacent communities
that have a high degree of economic and social integration within
the nucleus. Each MSA has one or more central counties containing
the area’s main population concentration. In New England,
metropolitan areas consist of cities and towns rather than whole
counties. Regions of residence are in accordance with the U.S.
Bureau of the Census definition.
Race/Ethnicity
Classification by race and ethnicity was based
on information reported for each household member. Respondents
were asked if their race was best described as American Indian,
Alaska Native, Asian or Pacific Islander, black, white, or other.
They were also asked if their main national origin or ancestry
was Puerto Rican; Cuban; Mexican, Mexicano, Mexican American, or
Chicano; other Latin American; or other Spanish. All persons who
claimed main national origin or ancestry in one of these Hispanic
groups, regardless of racial background, were classified as Hispanic.
Since the Hispanic grouping can include black Hispanic, white Hispanic,
and other Hispanic, the race categories of black, white, and other
do not include Hispanic.
Employment Status
Persons were considered to be employed if they
were age 16 and over, and had a job for pay, owned a business,
or worked without pay in a family business at the time of the Round
1 or Round 3 interview.
Sample
Design and Accuracy of Estimates
MEPS is designed to produce estimates at the
national and regional level over time for the civilian noninstitutionalized
population of the United States and some subpopulations of interest.
Each MEPS panel collects data covering a 2-year period, with the
first two MEPS panels spanning 1996-97 and 1997-98, respectively.
In this report, data from the 1997 portion of the third round of
data collection for the MEPS Panel 1 sample are pooled with data
from the first round of data collection for the MEPS Panel 2 sample
(shaded portion of Figure A).
The statistics presented in this report are affected
by both sampling error and sources of nonsampling error, which
include nonresponse bias, respondent reporting errors, interviewer
effects, and data processing misspecifications. For a detailed
description of the MEPS survey design, the adopted sample design,
and methods used to minimize sources of nonsampling error, see
Cohen (1997) and Cohen, Monheit, Beauregard, et al. (1996). The
MEPS person-level estimation
Source: Center for Financing, Access,
and Cost Trends, Agency for Health Care Policy and Research.
weights include nonresponse adjustments and poststratification
adjustments to population estimates derived from the March 1997
Current Population Survey (CPS) based on cross-classifications
by region, MSA status, age, race/ethnicity, and sex.
Tests of statistical significance were used to
determine whether the differences between populations exist at
specified levels of confidence or whether they occurred by chance.
Differences were tested using Z-scores having asymptotic normal
properties at the 0.05 level of significance. Unless otherwise
noted, only statistical differences between estimates are discussed
in the text.
Panel 1
At its beginning in 1996, MEPS Panel 1 consisted
of a sample of 10,639 households, a nationally representative subsample
of the households responding to the 1995 National Health Interview
Survey (NHIS). The 1995 NHIS sampled households with Hispanic members
and households with black members at approximately 2.0 and 1.5
times the rate of other households, respectively. These oversampling
rates are also reflected in the MEPS sample of households.
The overall MEPS Panel 1 response rate at the
end of Round 3 (which collects data for the first part of 1997)
was 70.2 percent. This overall rate reflects response to the 1995
NHIS interview and the MEPS interviews for Rounds 1-3.
Panel 2
At its beginning in 1997, MEPS Panel 2 consisted
of a sample of 6,281 households, a nationally representative subsample
of the households responding to the 1996 NHIS. Like Panel 1, the
Panel 2 sample reflects the oversampling
of Hispanic and black households in NHIS. However, the sample design
for Panel 2 differed from that for Panel 1 because the following
policy-relevant groups (classified based on 1996 NHIS data) were
also oversampled to produce more reliable estimates for these groups:
- Adults (age 18 and over) with functional impairments
(difficulty with one or more activities of daily living).
- Children (under age 18) with limitations in
activity.
- Individuals aged 18-64 expected to incur high
medical expenditures in 1997.
- Individuals predicted to reside in low-income
households (below 200 percent of poverty level).
- Adults (age 18 and over) with health limitations
other than functional impairments (difficulty with one or more
instrumental activities of daily living).
The overall MEPS Panel 2 response rate at the
end of Round 1 (when data were collected for the first part of
1997) was 77.9 percent. This overall rate reflects response to
both the 1996 NHIS interview and the MEPS Round 1 interview.
Combined Panel Response
Each panel was given approximately equal weight
in the development of sampling weights to produce national estimates.
Therefore, a pooled response rate for the survey respondents in
this data set can be obtained by taking an average of the panel-specific
response rates. This pooled response rate for the combined panels
is 74.1 percent.
Rounding
Estimates presented in the tables were rounded
to the nearest 0.1 percent. Standard errors, presented in Tables
B-F, were rounded to the nearest 0.01. Population estimates in
Tables 1-4 and Table A were rounded to the nearest thousand. Therefore,
some of the estimates presented in the tables for population totals
of subgroups will not add exactly to the overall estimated population
total.
Comparisons
with Other Data Sources
Other Surveys
Because of methodological differences, caution
should be used when comparing these data with data from other sources.
For example, CPS measures persons who are uninsured for a full
year; NHIS measures persons who lack insurance at a given point
in time--the month before the interview. The CPS interview that
contains information on the health insurance status of the population
is conducted annually, and NHIS collects insurance data on a continuous
basis each year. In addition, unlike MEPS, CPS counts as insured
military veterans whose source of health care is the Department
of Veterans Affairs. CPS also counts children of adults covered
by Medicaid as insured. For these preliminary estimates, MEPS did
not consider these children insured unless their families reported
them as such.
1996 MEPS Data
Users interested in comparing the 1996 and 1997
MEPS health insurance estimates should be aware that the standard
errors presented in the tables do not account for the fact that
the estimates are not independent. By design, the 1996 MEPS panel
respondents are present in both the 1996 and 1997 sample populations.
Users should also be aware of questionnaire wording differences
in the Rounds 1 and 3 MEPS interviews. The questionnaire for the
Round 3 interviews includes reviews of previously reported sources
of health insurance coverage. Note that the 1996 estimates presented
in MEPS Research Findings Number 1 (Vistnes and Monheit, 1997)
are based on data obtained during the 1996 MEPS Round 1 interview,
while the 1997 estimates are based on interviews conducted in Round
1 of the 1997 MEPS panel as well as Round 3 of the 1996 MEPS panel.
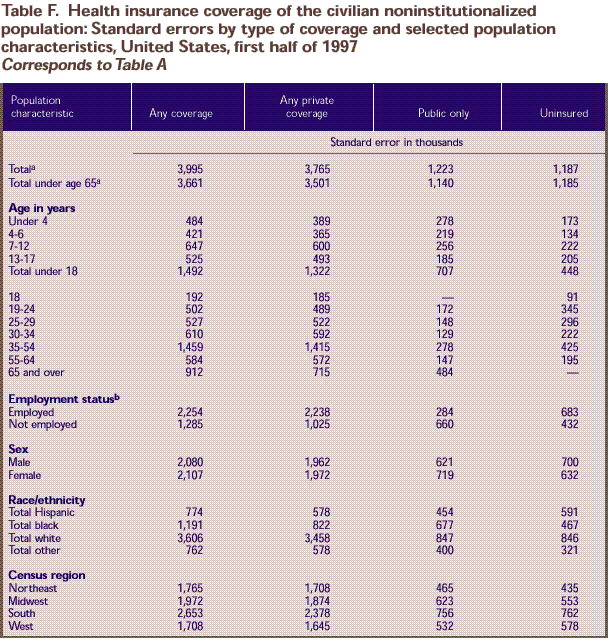
Population
and Standard Error Tables:
a Includes persons with unknown employment status.
b For individuals age 16 and over.
c Sample size too small to produce reliable estimates.
Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
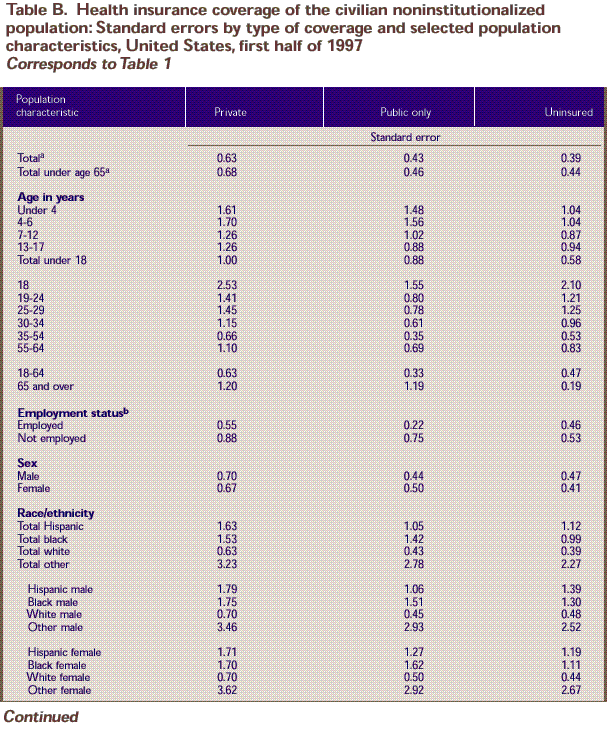
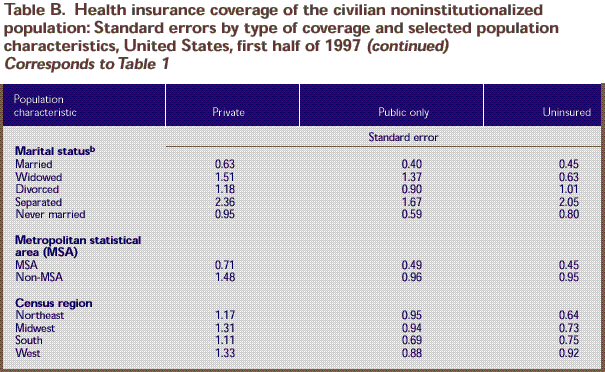
a Includes persons with unknown employment status
and marital status.
b For individuals age 16 and over. Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
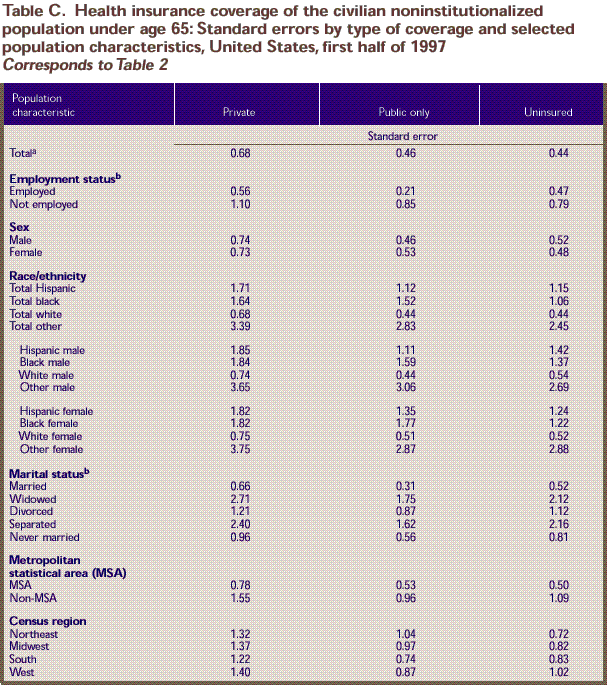
a Includes persons with unknown employment status
and marital status.
b For individuals age 16 and over. Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
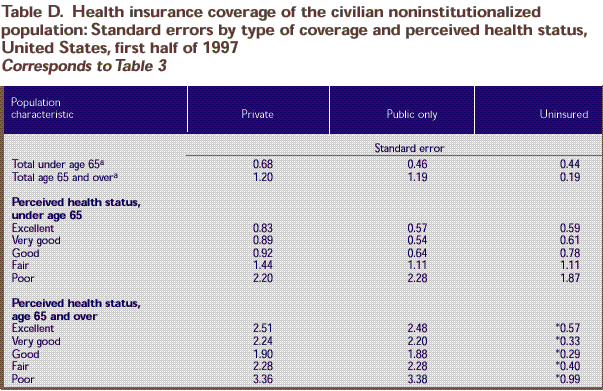
a Includes persons with unknown perceived health
status.
* Relative standard error is greater than or
equal to 30 percent. Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
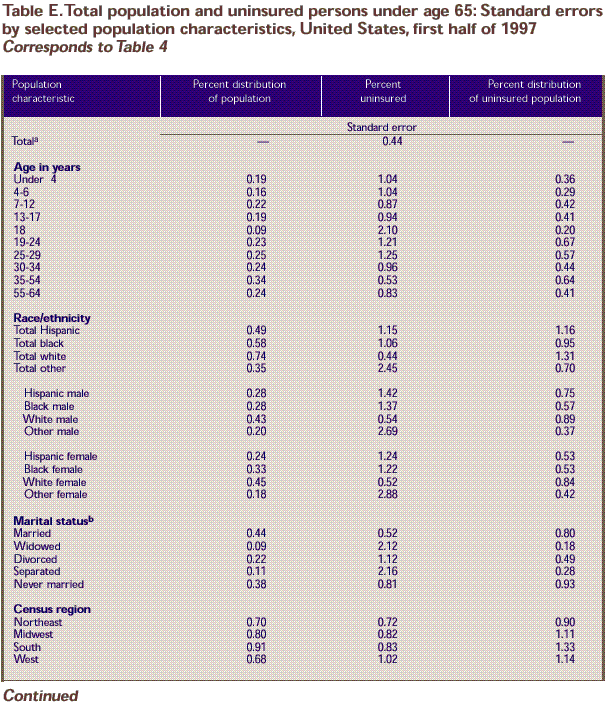
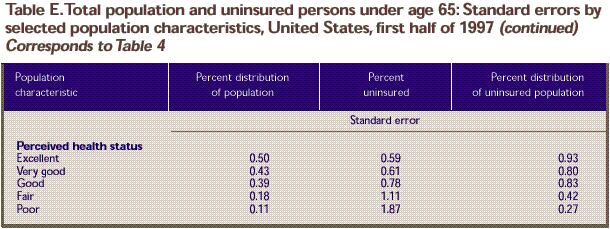
a Includes persons with unknown marital status
and perceived health status.
b For individuals age 16 and over.
Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
a Includes persons with unknown employment status.
b For individuals age 16 and over.
– Sample size
too small to produce reliable estimates.
Source: Center
for Financing, Access, and Cost Trends, Agency for Health Care
Policy and Research: Medical Expenditure Panel Survey Household
Component, 1997.
^top
Suggested
Citation:
Vistnes, J. P. and Zuvekas,
S. H. Research Findings #8: Health Insurance Status of the Civilian Noninstitutionalized Population, 1997. July 1999. Agency
for Healthcare Research and Quality, Rockville,
MD.
http://www.meps.ahrq.gov/data_files/publications/rf8/rf8.shtml |
| 