Methodology Report #19:
Overview of Methodology for Imputing Missing Expenditure Data in the Medical Expenditure Panel Survey
Steven R. Machlin, Agency for Healthcare Research and Quality,
and Deborah D. Dougherty, Westat.
Table of Contents
Abstract
The Medical Expenditure Panel Survey (MEPS)
Introduction
MEPS Sample Design
MEPS Expenditures Defined
MEPS Household Expenditure Data Collection
MEPS Expenditure Estimation Strategy
Imputation Process
Summary
References
Acknowledgments
Abstract
In the Medical Expenditure Panel Survey (MEPS), expenditures are defined as payments
from all sources (including individuals, private insurance, Medicare, Medicaid, and
other sources) for health care services during the year. Data on expenditures are
collected for sample persons in the Household Component of the survey and from a
sample of their health care providers responding to the Medical Provider Component of
the survey. In the absence of payment information from either component, expenditure
data are completed through weighted hot-deck imputation procedures. The MEPS collects
a wide variety of data about indivi-duals and health care events that are correlated
with expenditures and, for each event type (e.g., doctor visits, hospitalizations, etc.),
a selected set of these variables is used in the imputation processes. Several hot-deck
iterations are run for each medical event type category based on factors such as whether
partial payment information was reported and whether payments for the event covered
multiple visits. This paper provides an overview of the methodological approach to
impute MEPS expenditure data and how class variables for the hot-deck procedures were
determined.
The estimates in this report are based on the most recent data available at the time
the report was written. However, selected elements of MEPS data may be revised on the
basis of additional analyses, which could result in slightly different estimates from
those shown here. Please check the MEPS Web site for the most current file releases.
Center for Financing, Access, and Cost Trends
Agency for Healthcare Research and Quality
540 Gaither Road
Rockville, MD 20850
http://www.meps.ahrq.gov/
The Medical Expenditure Panel Survey (MEPS)
Background
The Medical Expenditure Panel Survey (MEPS) is conducted
to provide nationally representative estimates of health care use,
expenditures, sources of payment, and insurance coverage for the U.S.
civilian noninstitutionalized population. MEPS is cosponsored by the
Agency for Healthcare Research and Quality (AHRQ), formerly the Agency
for Health Care Policy and Research, and the National Center for Health
Statistics (NCHS).
MEPS comprises three component surveys: the Household
Component (HC), the Medical Provider Component (MPC), and the Insurance
Component (IC). The HC is the core survey, and it forms the basis for
the MPC sample and part of the IC sample. Together these surveys yield
comprehensive data that provide national estimates of the level and
distribution of health care use and expenditures, support health
services research, and can be used to assess health care policy
implications.
MEPS is the third in a series of national probability
surveys conducted by AHRQ on the financing and use of medical care in
the United States. The National Medical Care Expenditure Survey (NMCES)
was conducted in 1977, the National Medical Expenditure Survey (NMES) in
1987. Beginning in 1996, MEPS continues this series with design
enhancements and efficiencies that provide a more current data resource
to capture the changing dynamics of the health care delivery and
insurance system.
The design efficiencies incorporated into MEPS are in
accordance with the Department of Health and Human Services (DHHS)
Survey Integration Plan of June 1995, which focused on consolidating
DHHS surveys, achieving cost efficiencies, reducing respondent burden,
and enhancing analytical capacities. To accommodate these goals, new
MEPS design features include linkage with the National Health Interview
Survey (NHIS), from which the sample for the MEPS-HC is drawn, and
enhanced longitudinal data collection for core survey components. The
MEPS-HC augments NHIS by selecting a sample of NHIS respondents,
collecting additional data on their health care expenditures, and
linking these data with additional information collected from the
respondents’ medical providers, employers, and insurance providers.
Household Component
The MEPS-HC, a nationally representative survey of the
U.S. civilian noninstitution-alized population, collects medical
expenditure data at both the person and household levels. The HC
collects detailed data on demographic characteristics, health
conditions, health status, use of medical care services, charges and
payments, access to care, satisfaction with care, health insurance
coverage, income, and employment.
The HC uses an overlapping panel design in which data
are collected through a preliminary contact followed by a series of five
rounds of interviews over a two and a half year period. Using
computer-assisted personal interviewing (CAPI) technology, data on
medical expenditures and use for two calendar years are collected from
each household. This series of data collection rounds is launched each
subsequent year on a new sample of households to provide overlapping
panels of survey data and, when combined with other ongoing panels, will
provide continuous and current estimates of health care expenditures.
The sampling frame for the MEPS-HC is drawn from
respondents to NHIS, conducted by NCHS. NHIS provides a nationally
representative sample of the U.S. civilian noninstitutionalized
population, with oversampling of Hispanics and blacks.
Medical Provider Component
The MEPS-MPC supplements and validates information on
medical care events reported in the MEPS-HC by contacting medical
providers and pharmacies identified by house-hold respondents. The MPC
sample includes all hospitals, hospital physicians, home health
agencies, and pharmacies reported in the HC. Also included in the MPC
are all office-based physicians:
- Providing care for HC respondents
receiving Medicaid.
- Associated with a 75 percent sample of
households receiving care through an HMO (health maintenance
organization) or managed care plan.
- Associated with a 25 percent sample of
the remaining households. Data are collected on medical and
financial characteristics of medical and pharmacy events reported by
HC respondents, including:
- Diagnoses coded according to ICD-9 (9th
Revision, International Classification of Diseases) and DSMIV
(Fourth Edition, Diagnostic and Statistical Manual of Mental
Disorders).
- Physician procedure codes classified by
CPT-4 (Current Procedural Terminology, Version 4).
- Inpatient stay codes classified by DRG
(diagnosis related group).
- Prescriptions coded by national drug code
(NDC), medication names, strength, and quantity dispensed.
- Charges, payments, and the reasons for
any difference between charges and payments.
The MPC is conducted through telephone interviews and
mailed survey materials.
Insurance Component
The MEPS-IC collects data on health insurance plans
obtained through private and public sector employers. Data obtained in
the IC include the number and types of private insurance plans offered,
benefits associated with these plans, premiums, contributions by
employers and employees, and employer characteristics.
Establishments participating in the MEPS-IC are selected
through three sampling frames:
- A list of employers or other insurance
providers identified by MEPS-HC respondents who report having
private health insurance at the Round 1 interview.
- A Bureau of the Census list frame of
private-sector business establishments.
- The Census of Governments from the
Bureau of the Census.
To provide an integrated picture of health insurance,
data collected from the first sampling frame (employers and other
insurance providers) are linked back to data provided by the MEPS-HC
respondents. Data from the other three sampling frames are collected to
provide annual national and State estimates of the supply of private
health insurance available to American workers and to evaluate
policy issues pertaining to health insurance. Since 2000, the Bureau of
Economic Analysis has used national estimates of employer contributions
to group health insurance from the MEPS-IC in the computation of Gross
Domestic Product (GDP).
The MEPS-IC is an annual panel survey. Data are
collected from the selected organizations through a prescreening
telephone interview, a mailed questionnaire, and a telephone follow-up
for nonrespondents.
Survey Management
MEPS data are collected under the authority of the
Public Health Service Act. They are edited and published in accordance
with the confidentiality provisions of this act and the Privacy Act.
NCHS provides consultation and technical assistance.
As soon as data collection and editing are completed,
the MEPS survey data are released to the public in staged releases of
summary reports and microdata files. Summary reports are released as
printed documents and electronic files. Microdata files are released on
CD-ROM and/or as electronic files.
Printed documents and CD-ROMs are available through the
AHRQ Publications Clearinghouse. Write or call:
AHRQ Publications Clearinghouse
Attn: (publication number)
P.O. Box 8547 Silver Spring, MD 20907
800-358-9295
703-437-2078 (callers outside the United States only)
888-586-6340 (toll-free TDD service; hearing impaired only)
To order online, send an e-mail to: ahrqpubs@ahrq.gov.
Be sure to specify the AHRQ number of the document or
CD-ROM you are requesting. Selected electronic files are available
through the Internet on the MEPS Web site:
http://www.meps.ahrq.gov/
For more information, visit the MEPS Web site or e-mail
mepspd@ahrq.gov.
Return to Table of Contents
Table of Contents
Abstract
The Medical Expenditure Panel Survey (MEPS)
Introduction
MEPS Sample Design
MEPS Expenditures Defined
MEPS Household Expenditure Data Collection
MEPS Expenditure Estimation Strategy
Imputation Process
Summary
References
Acknowledgments
Introduction
The Medical Expenditure Panel Survey (MEPS) is a complex national probability survey of the U.S.
civilian noninstitutionalized population, and has been conducted on an annual basis since 1996 by
the Agency for Healthcare Research and Quality (AHRQ). One of the primary purposes of the survey
is to collect data that can be used to analyze national medical expenditures (i.e., the amount paid
for health care services).
Unfortunately, it is difficult to obtain complete information on medical expenditures from household
survey respondents because the type of information being collected is often not straightforward and
requires extensive record keeping over time, especially for households with members who frequently
use the health care system. Further, in a significant number of instances, respondents are simply not
aware of either the total amount billed or how much the provider is paid for the services that were
received. Classic examples are individuals enrolled in the Medicaid program, where financial transactions
occur only between the provider and the state Medicaid agency, and enrollees of managed care plans or
HMOs who only may be aware of paying some predetermined co-payment that is not necessarily related to
the total amount the provider receives (Cohen et al., 1997).
As a consequence of these factors, there is a substantial amount of item nonresponse on medical expenses
in the Household Component (HC) of MEPS. To compensate for these missing data and to improve accuracy,
data on expenses for sample persons are also collected from a sample of their health care providers in
the Medical Provider Component (MPC) of MEPS (see description of MPC under MEPS Expenditure Estimation
Strategy below). However, expense data are not available from either survey component for a noteworthy
proportion of medical events reported in the survey (e.g., roughly one-third in 2001).
A weighted hot-deck approach is used to impute missing expenditure data in MEPS. This approach uses other
survey responses to complete missing data and incorporates survey weights to replicate the weighted
distribution of the available data in the imputed data (Cox, 1980). The objectives of the imputations
are to create data sets for analysis that preserve sample sizes and reduce the potential for nonresponse
bias in analyses of MEPS expenditure data. This paper provides a general overview of the MEPS expenditure
imputation process.
Return to Table of Contents
MEPS Sample Design
The sample of households for the MEPS-HC is a subsample of households that responded to the prior year’s
National Health Interview Survey (NHIS) conducted by the National Center for Health Statistics (National
Center for Health Statistics, 2002). The MEPS sample is drawn from approximately half of the primary
sampling units (PSUs) selected for the NHIS. For example, the 1996 MEPS-HC sample was selected from
households that responded to the 1995 NHIS (Cohen S., 1997). This selection was comprised of 195 PSUs and
1,675 sample segments (second-stage sampling units). Over sampling of households with Hispanics and blacks
carries over from the NHIS to the MEPS sample design.
The sample design of the Medical Expenditure Panel Survey is an
overlapping panel design, with data collected for each new MEPS panel covering a two-year period (Cohen J., 1997).
As a result of the overlapping panel design, MEPS annual data for 1997 and beyond are constructed based on data
collected from two consecutive panels.
Return to Table of Contents
MEPS Expenditures Defined
Total medical expenditures in MEPS are defined as the
sum of direct payments for care provided during the year, including
out-of-pocket payments and payments by third-party payers (e.g., private
insurance, Medicare, Medicaid, and other sources), rather than the
amount billed by the provider for the care provided (i.e., charges).
Payments for hospital and physician services, ambulatory physician and
nonphysician services, prescribed medicines, home health services,
dental services, and various other medical equipment and services that
were purchased or rented during the year are included. Payments for
over-the-counter drugs and phone contacts with providers are not
collected in MEPS.
Provider charges for health care are not considered a
proxy for payments, primarily due to two important trends that have
occurred since the mid 1990s (Zuvekas and Cohen, 2002). First, pressure
to contain health care costs by employers has increased insurers’
leverage to negotiate substantial discounts with providers. Second, the
insurance industry made significant movement toward capitation as a way
of increasing the incentive for providers to contain costs by being
subjected to financial risk for high levels of utilization. As a result,
for a sizeable number of medical events, charges have become virtually
meaningless as a measure of payments. Nevertheless, charges are
collected in MEPS because they are highly correlated with payments and
are incorporated in the imputation process for missing expenditure data
wherever possible (see Example 3 below).
Return to Table of Contents
MEPS Household Expenditure Data Collection
Primary data collection in the MEPS-HC employs
computer-assisted personal interviewing (CAPI). The HC questionnaire is
designed to collect use and expenditure data for two consecutive years
through a series of five interviews. In general, annual health care
utilization and expenses for sample persons are derived from information
collected in three of the five interviews (Cohen J., 1997).
Figure 1 provides a pictorial summary of the data
collection process for medical events and expenses in MEPS. For each
person in a sample household, the core instrument collects detailed data
about medical care received as well as charges and payments for each
health care event reported in the utilization section. Medical events
reported are grouped into the following categories: office-based medical
provider visits, hospital emergency room visits, hospital outpatient
visits, hospital inpatient stays, dental visits, home health, prescribed
medicines, and other medical expenses. Payments for each event are
itemized according to the following 10 source of payment categories: out
of pocket, Medicare, Medicaid, private insurance, Veteran’s
Administration, TRICARE, Other Federal sources, Other State and local sources,
Workers’ Compensation, and Other unclassified sources. Payments for a
particular medical event can be made across one or a combination of sources
(though total payments for a small proportion of events each year are considered
to be $0, which occurs when it is reported that no payments were or will
be made). Total expenses for a given event are obtained by summing
across all payment sources.
Figure 1. Illustration of collection of medical event and source of payment data: MEPS
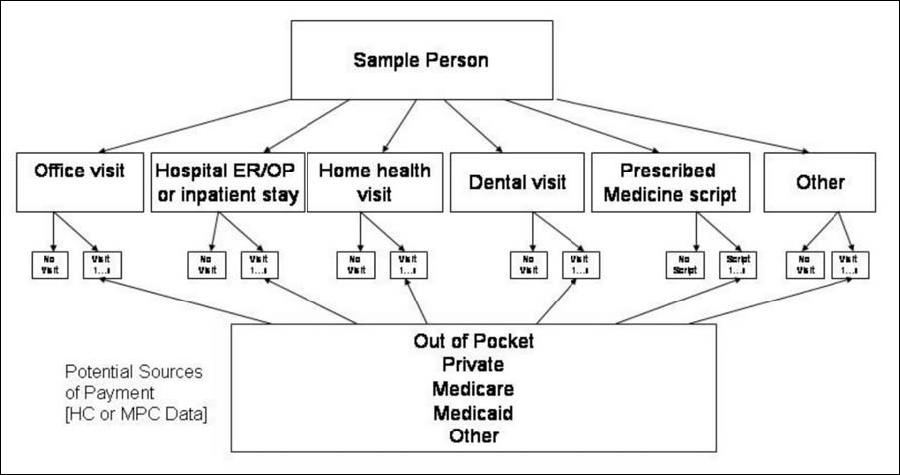
Nonresponse on payments for a particular medical event
may occur for any potential payment source. However, it is not unusual
for respondents to report the amount paid out of pocket and that a
third-party source(s) paid an unknown amount (i.e., partial item nonresponse).
Return to Table of Contents
MEPS Expenditure Estimation Strategy
In addition to the HC, MEPS expenditure data are also
collected in the Medical Provider Component (MPC) of the survey. The
purpose of the MPC is to collect data directly from a sample of medical
providers to reduce the level of missing data and to improve the
accuracy of expenditure estimates that would be obtained by relying
solely on household responses (Machlin and Taylor, 2000, and Cohen J. et
al., 1997). Data from the MPC are considered to be more accurate on
average than comparable data reported by household respondents in the HC.
Data obtained in the MPC are linked to medical events
reported in the HC based on a probabilistic matching procedure (Winglee
et al., 1999). As a consequence of the matching process, each medical
event reported in the HC will have expense data from both the HC and MPC,
one of these sources, or neither source (i.e., complete missing payment
data). A hierarchical approach is used to develop complete data for
expenditures as follows: 1) start with household reported medical
events, 2) use MPC expense data where available, 3) use HC expense data
if no MPC data available, and 4) impute any missing information. Table 1
shows the distribution by source of expenditure data (i.e., HC, MPC, or
imputed) in 2001 for each type of event category, and the subsequent
discussion provides an overview of the imputation process.
Table 1. Distribution of source of expenditure data for survey-reported health care events, by type of service, 2001 MEPS
| |
|
Hospital events |
|
|
| |
Office visits |
Outpatient visits |
Emergency room visits |
Inpatient stays |
Dental visits1 |
Home health2 |
| Number of events |
142,793 |
15,763 |
5,904 |
3,405 |
26,438 |
3,155 |
|
Percent distribution by source of data3 |
| Total |
100.0 |
100.0 |
100.0 |
100.0 |
100.0 |
100.0 |
| MPC |
27.9 |
46.7 |
47.9 |
61.4 |
-- |
42.3 |
| HC |
17.5 |
6.2 |
8.1 |
3.7 |
47.1 |
9.4 |
| Imputed: Partial4 |
19.2 |
8.2 |
9.7 |
4.9 |
11.8 |
0.1 |
| Imputed: Full |
35.3 |
38.9 |
34.3 |
30.0 |
41.1 |
48.2 |
1
Dental care providers are not surveyed in the MEPS Medical Provider Component, so MPC
category is not applicable.
2
Expense data for home health are collected on a monthly rather than a per visit basis.
3
Percentages for office visits do not add to exactly 100.0 due to rounding.
4
Includes events where expense information was imputed for some but not all payment sources.
Return to Table of Contents
Imputation Process
Separate imputations are conducted for each event type
category because relevant variables and statistically significant
correlates of expenditures vary by type of event. However, insurance
coverage is utilized for all imputations regardless of event type
because generosity of payments is associated with type of coverage. For
example, Medicaid payments are typically less generous than private
insurance payments for comparable services.
Missing expenditure data for health care events reported
in the survey are completed through a weighted hot-deck imputation
procedure (Cox, 1980), with data from the MPC used as the primary donor
source wherever possible. In general, the hot-deck procedure sorts donor
events (complete data) and recipient events (missing data) into
imputation cells based on important predictors of expenses available in
MEPS. For example, the imputation procedure for hospital inpatient
events sorts donors and recipients into cells based on insurance
coverage of the sample person, number of nights in the hospital, reason
for hospitalization, whether the hospital admission immediately followed
an emergency room visit, as well as region and urbanization level of the
person’s residence. Whenever possible, a donor is selected within the
same cell as a recipient to complete a recipient record. However, if
there are fewer donors than recipients in a cell, cells are collapsed in
a predetermined order until a 1:1 ratio of donors to recipients is
achieved. In general, the order used for cell collapsing is determined
based on the relative strength of the associations between the
classification variables and expenses.
Imputations are handled somewhat differently depending
on 1) whether all or some potential sources of payment are missing and
2) whether the total charge for the event was reported or not. Following
are examples of three different scenarios for imputation of hospital
inpatient expenses. These examples assume that donors and recipients
match on the pertinent correlates of expenditures (e.g., insurance
coverage, number of nights in the hospital, reason for hospitalization,
whether the hospital admission immediately followed an emergency room
visit, region, and urbanization).
Example 1. Complete imputation
| Payment source |
Donor |
Recipient (pre-imputation) |
Recipient (post-imputation) |
| Medicare |
$1,840 |
Missing |
$1,840 |
| Private insurance |
$792 |
Missing |
$792 |
| Total expenses |
$2,632 |
-- |
$2,632 |
In Example 1, it was reported that a sample person had a
hospital inpatient stay and was covered by Medicare and private
insurance but the respondent did not know the amount paid by either
source for that stay. The donor record that was selected for this
recipient in the hot-deck procedure was an inpatient stay where the
hospital was paid a total of $2,632, of which $1,840 was from Medicare
and $792 was from a supplemental private insurance policy. These
identical values were imputed to the recipient record.
Example 2. Partial imputation
| Payment source |
Donor |
Recipient (pre-imputation) |
Recipient (post-imputation) |
| Out of pocket |
$26 |
$5 |
$5 |
| Private insurance |
$971 |
Missing |
$992 |
| Total expenses |
$997 |
-- |
$997 |
In Example 2, it was reported that a sample person had
an inpatient hospitalization, was covered by private insurance, and that
$5 was paid out of pocket but the respondent did not know the amount
paid to the hospital by private insurance. The donor record that was
selected for this recipient in the hot-deck procedure was an inpatient
stay where the hospital was paid a total of $997, of which $26 was paid
out of pocket and $971 was from private insurance. In this situation,
the total amount paid for the event from the donor ($997) was imputed to
the recipient record, the reported out-of-pocket amount ($5) was
retained, and the difference ($992) was imputed to the recipient record
as a private insurance payment.
Example 3. Imputation using total charge
| Payment source |
Donor |
Recipient (pre-imputation) |
Recipient (post-imputation) |
| Total charges |
$5,171 |
$4,173 |
$4,173 |
| Total expenses |
$4,248 |
missing |
$3,421 |
| Medicare |
$3,411 |
missing |
$2,737 |
| Private insurance |
$837 |
missing |
$684 |
As described earlier (see section on MEPS Expenditures
Defined), charges are not identical to but are highly correlated with
expenditures (payments) made for health care. In most instances, when
there are missing data on payments for a health event reported in the
survey there are also missing data on charges. However, in situations
where the respondent reports the total charge for an event but does not
know the actual payments, the reported information on charges is used to
improve the accuracy of the imputation.
To illustrate the use of total charge information when
available, in Example 3 the respondent reported there was $4,173 in
hospital facility charges for the reported inpatient stay. The donor
record selected for the imputation in the hot-deck procedure showed
$5,171 in total charges and $4,248 in total expenses. The first step
imputes total expenses to the recipient record by applying the ratio of
total expenses to total charges on the donor record (4,248/5,171) to the
total charges on the recipient record ($4,173). Then, the imputed total
expense on the recipient record ($3,421) is allocated across the two
potential sources of payment, Medicare and private insurance, in the
same proportion as on the donor record (i.e., 837/4,248 and 3411/4,248
for Medicare and private insurance, respectively).
Return to Table of Contents
Summary
MEPS is an ongoing survey that collects data on the
utilization and expenditures for health care in the U.S. civilian
noninstitutionalized population. Given the complexity of the U.S. health
care system and the wide range of public and private financing
arrangements, it is difficult to collect complete information on health
care expenses.
To maximize the completeness and accuracy of expenditure
data, MEPS integrates data on utilization and expenditures from the
Household Component of the survey with data from a sample of providers
that participate in the Medical Provider Component of the survey. To
complete medical expenditure data that were not obtained from either
component, a weighted hot-deck imputation procedure is used. The primary
advantage of this procedure is that the distribution of data values
(including the imputed ones) will look similar to the distribution of
the values in the population (Korn and Graubard, 1999).
The hot-deck procedures used to complete missing
expenditure data in MEPS are based on statistical as well as substantive
considerations regarding the U.S. health care financing system. For
example, type of health insurance coverage is used as an auxiliary
variable in the imputations for all health service type categories
because of differences in average payments between insured and uninsured
persons as well as varying generosity of payments by type of insurance
coverage. In contrast, length of stay is incorporated as a
classification variable in the hot deck only for inpatient stays because
it is significantly associated with expenditures for hospital inpatient
stays, but is irrelevant when imputing expenses for other types of
health care events.
In summary, the dual objectives of imputing missing
expenditure data in MEPS are to maximize sample sizes available for
analysis and to reduce the risk of nonresponse bias associated with
exclusion of cases with missing data. However, the imputation approach
used is inherently complex, resource intensive, and leads to
underestimation of variances for survey estimates without an additional
correction. While it is difficult to assess the impact of imputation on
variances, the Center for Financing, Access, and Cost Trends at AHRQ is
currently conducting methodological research to estimate the magnitude
of the impact. Results of a preliminary investigation of the impact of
the expenditure imputations in MEPS have been reported (Baskin, 2004).
Return to Table of Contents
References
Baskin, R., Wun, L., Sommers, J., et al. Investigation
of the impact of imputation on variance estimation in the Medical
Expenditure Panel Survey. American Statistical Association 2004 Proceedings.
2004.
Cohen, J. Design and Methods of the Medical Expenditure Panel
Survey Household Component. MEPS Methodology Report No. 1. AHCPR Pub. No.
97-0026. Rockville, Md.: Agency for Health Care Policy and Research, 1997.
Cohen, J., Monheit, A., Cohen, S., et al. The Medical
Expenditure Panel Survey: A National Health Information Resource. Inquiry,
33: 373-389 (Winter 1996/97).
Cohen, S. Sample Design of the 1996 Medical Expenditure Panel Survey Household Component.
MEPS Methodology Report No. 2. AHCPR Pub. No.
97-0027. Rockville, Md.: Agency for Health Care Policy and Research, 1997.
Cox, B. The weighted sequential hot deck imputation
procedure. American Statistical Association 1980 Proceedings of the Section on
Survey Research Methods, 721-726. 1980.
Korn, E. and Graubard, B. Analysis of Health Surveys.
Wiley Series in Probability and Statistics. 1999.
Machlin, S. and Taylor, A. Design, Methods, and Field Results of the 1996
Medical Expenditure Panel Survey Medical Provider Component.
MEPS Methodology Report No.9. AHRQ Pub. No.00-0028. Rockville, Md.: Agency for
Healthcare Research and Quality, 2000.
National Center for Health Statistics. Health, United
States, 2002 (361-362). Hyattsville, Md.: 2002.
Winglee, M., Valliant, R., Brick, M., and Machlin, S. Probability matching of
medical events. Journal of Economic and Social Measurement 23 (1999)
1-12.
Zuvekas, S. H. and Cohen, J. W. A guide to comparing
health care expenditures in the 1996 MEPS to the 1987 NMES. Inquiry,
Spring 2002; 39:76-86.
Return to Table of Contents
Acknowledgments
The authors wish to thank Trena Ezzati-Rice, Joel Cohen, and Steven Cohen for their
helpful reviews of the paper.
Return to Table of Contents
Return to the MEPS Homepage
Suggested Citation:
Machlin, S. R. and Dougherty, D. D. Overview of Methodology for Imputing Missing Expenditure Data
in the Medical Expenditure Panel Survey. Method-ology Report No. 19. March 2007.
Agency for Healthcare Research and Quality, Rockville, Md. http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr19/mr19.shtml |
