Skip to main content
|
||||||||||||||||||
|
|
||||||||||||||||||
STATISTICAL BRIEF #542:
|
||||||||||||||||||
| March 2022 | ||||||||||||||||||
|
Asako S. Moriya, PhD and Zhengyi Fang, MS
|
||||||||||||||||||
Highlights
|
||||||||||||||||||
IntroductionPrescription opioids have commonly been used to treat both chronic and acute pain in the United States despite the fact that they are not recommended as the first-line treatment for most types of pain due to serious risks of opioid use disorders (OUDs) and overdose. As OUDs and opioid overdose deaths continue to be major public health concerns, examining the patterns and trends of the use of prescribed opioids can contribute to efforts to promote safer and more effective pain management.This Statistical Brief presents estimates of fills of prescriptions for opioid medications that are commonly used to treat pain obtained from the 2018-2019 Medical Expenditure Panel Survey Household Component (MEPS-HC). These estimates are an update of the 2015-2016 estimates presented in the previous Agency for Healthcare Research and Quality (AHRQ) Statistical Brief #516. The estimates only include prescriptions purchased or obtained in an outpatient setting. Prescription medicines administered in an inpatient setting or in a clinic or physician's office are not included. The sample includes all non-elderly adults (ages 18 to 64) in the U.S. civilian noninstitutionalized population. (Statistical Brief 541 presents estimates of opioid use for elderly adults ages 65 and older). We examine the average annual percentages of non-elderly adults in 2018-2019 with any opioid use (one or more prescription fills during the year) and with frequent opioid use, which we define as having five or more prescription fills or refills during the year. We present overall estimates for the full population of non-elderly adults and for subgroups defined by sex, race/ethnicity, poverty status, insurance coverage, perceived health status, Census region, and metropolitan statistical area (MSA) status. All differences mentioned in the text are significant at the .05 level or better. Because of methodological and definitional differences, readers should use caution when comparing Medical Expenditure Panel Survey (MEPS) data with data from other sources. Details on the MEPS methodology and differences from other sources are included in the Definitions section of this Statistical Brief. |
||||||||||||||||||
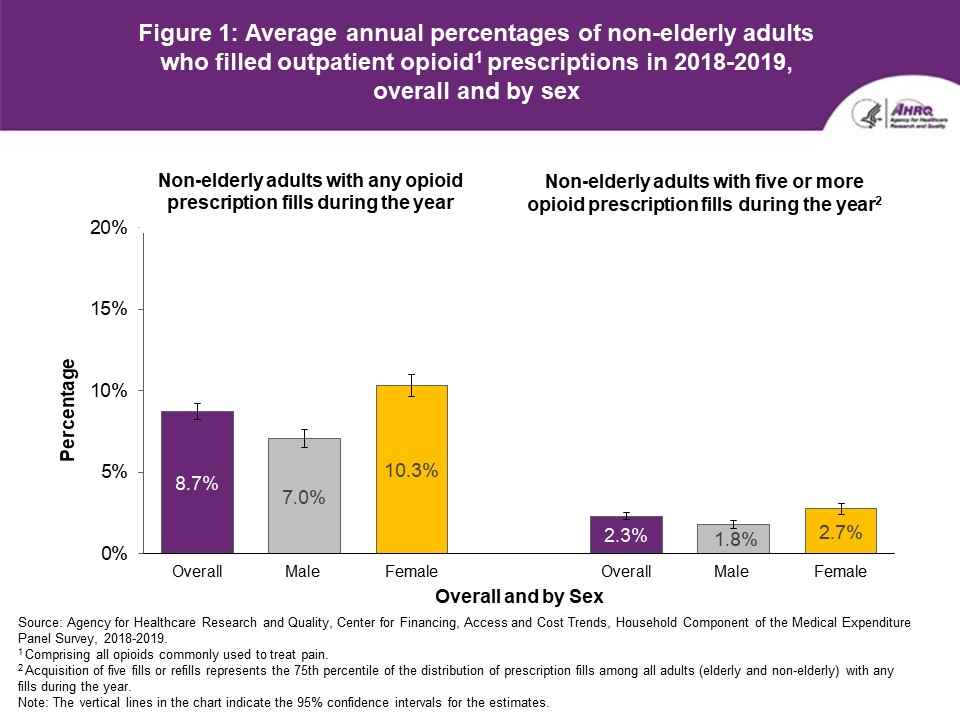
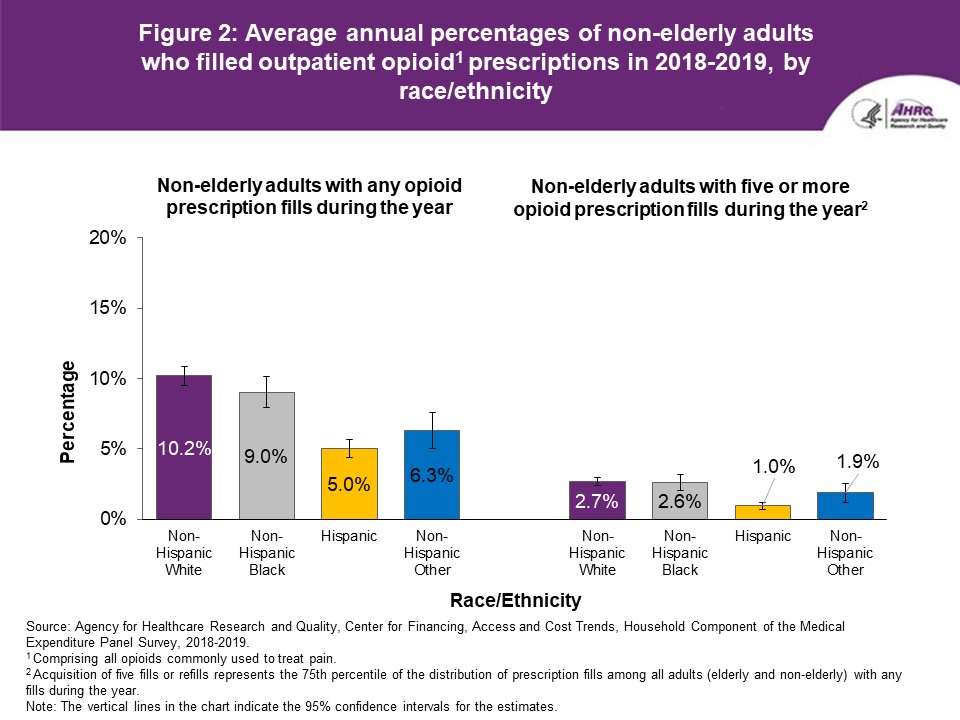
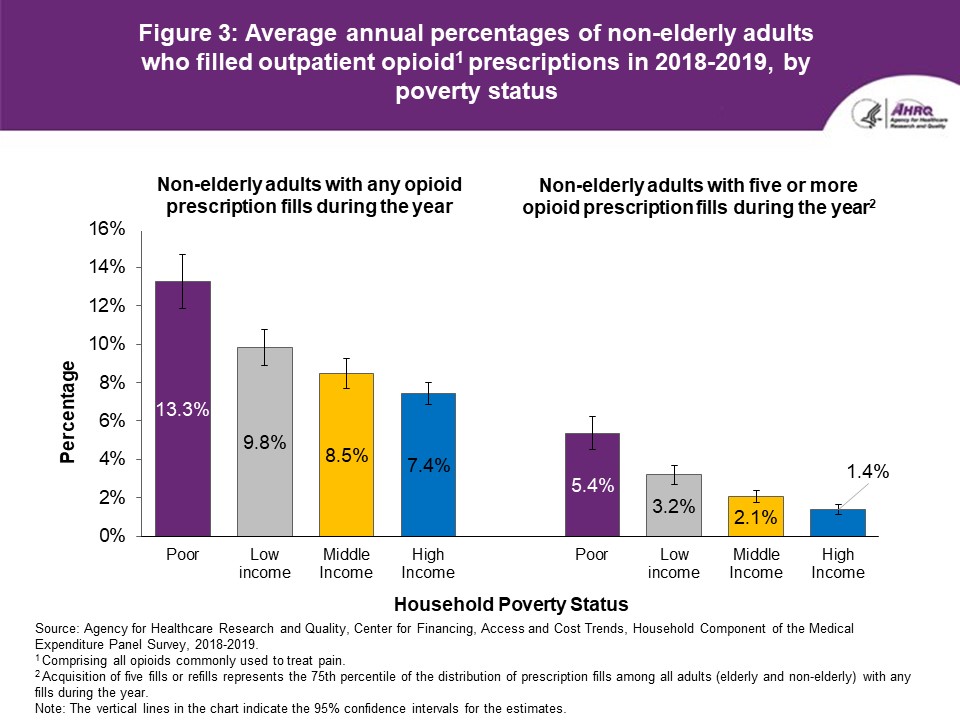
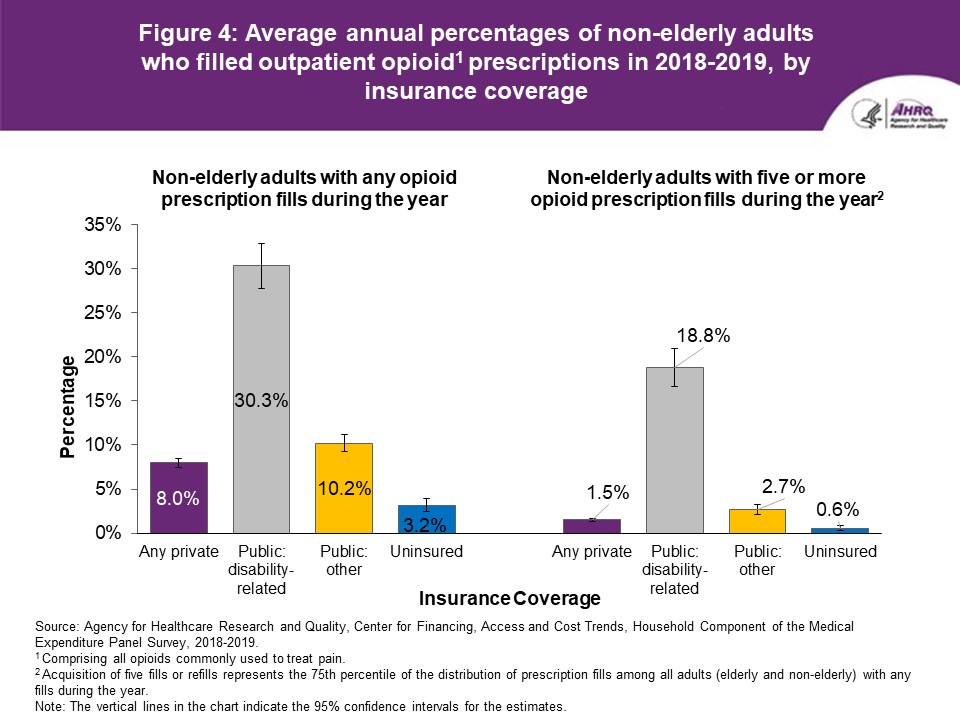
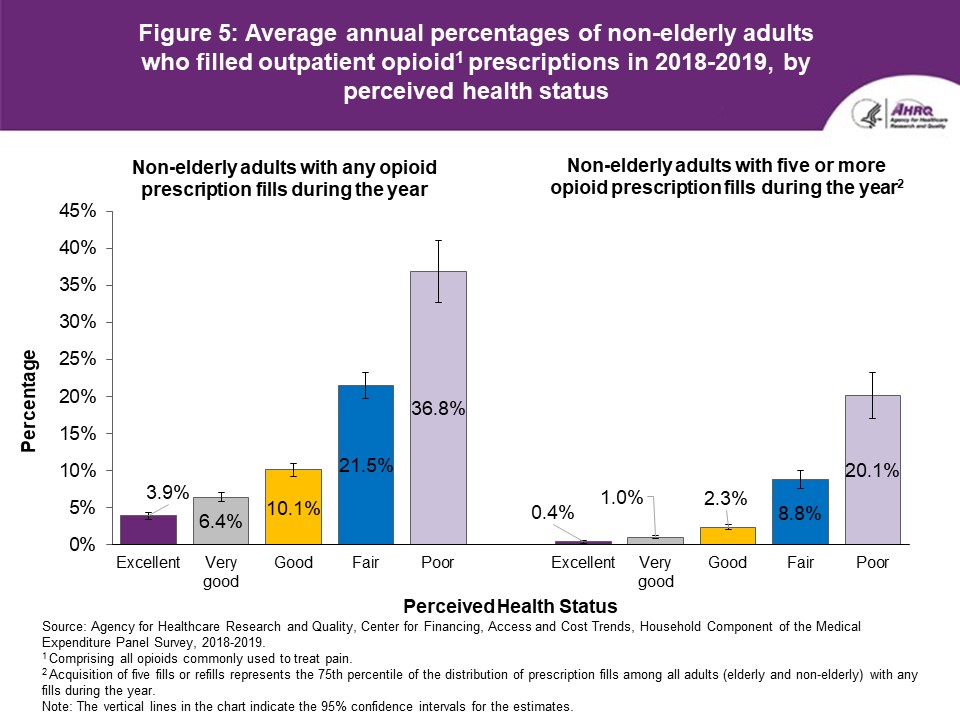
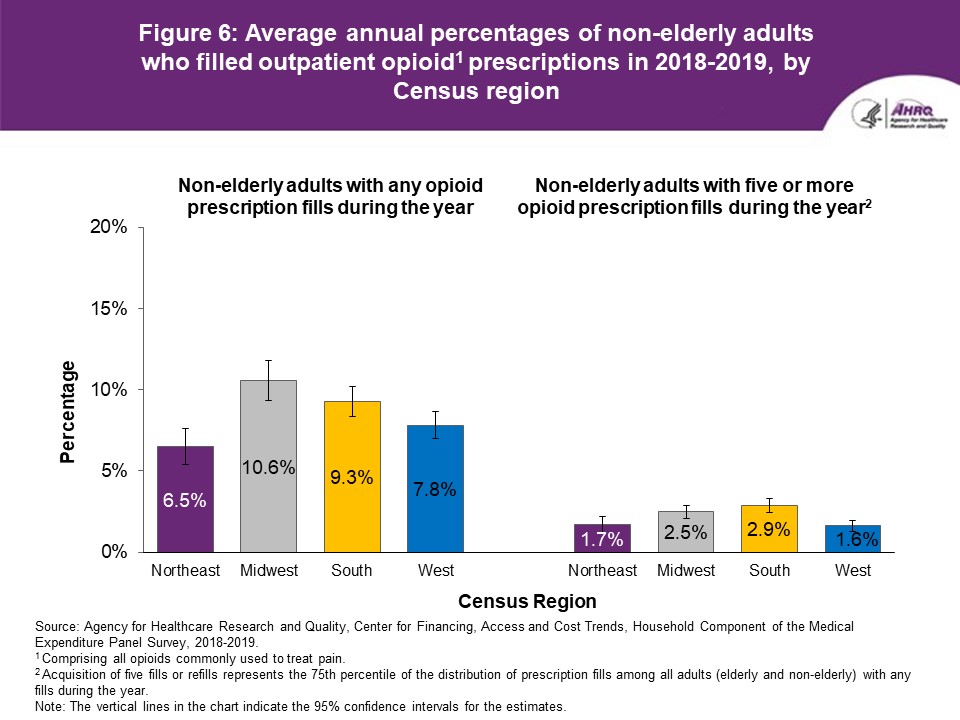
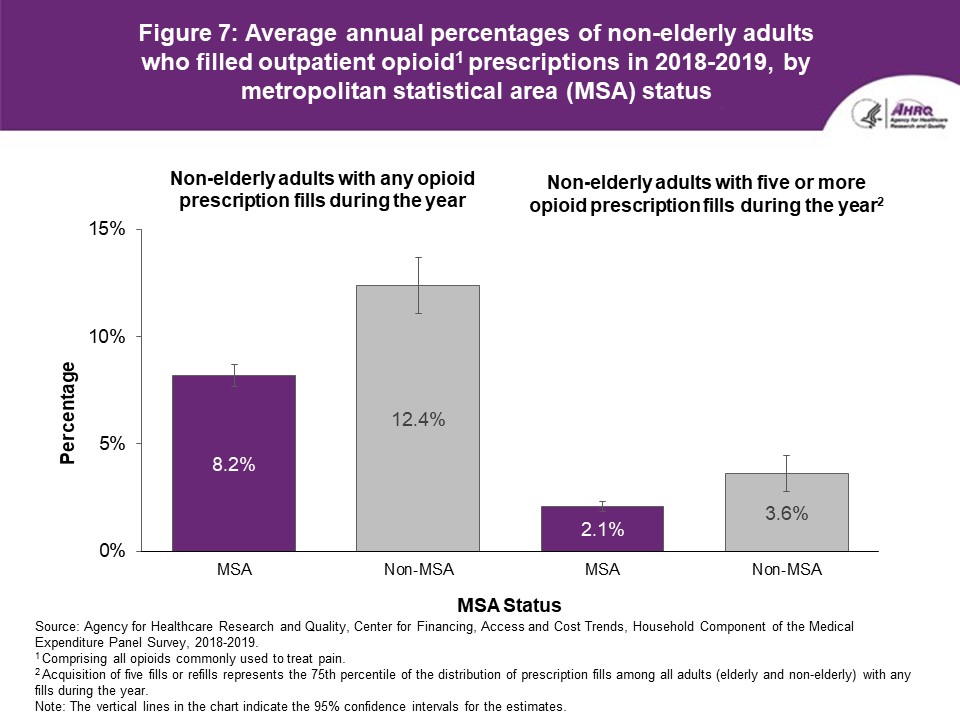
FindingsOverall and sex (figure 1)In 2018-2019, an average annual total of 17.3 million non-elderly adults, or 8.7 percent of the 198.4 million non-elderly adults in the U.S. civilian noninstitutionalized population, filled at least one opioid prescription during the year, and 4.5 million (2.3 percent) obtained five or more prescription fills (figure 1). Women were more likely than men to have any opioid use during the year (10.3 percent vs. 7.0 percent) and to have frequent opioid use (2.7 percent vs. 1.8 percent). Race/ethnicity (figure 2) In 2018-2019, the average annual percentage of those with at least one opioid prescription fill during the year was higher for non-Hispanic White non-elderly adults (10.2 percent) than for non-elderly adults in any of the other race/ethnicity categories (figure 2; the difference between non-Hispanic White and Black adults was significant at the p < 0.10 level). Non-Hispanic Black non-elderly adults (9.0 percent) were more likely to fill at least one opioid prescription than Hispanic adults (5.0 percent) and individuals of other races (6.3 percent). The average annual percentage of non-elderly adults who had at least five opioid prescription fills during the year was higher for non-Hispanic White (2.7 percent) and non-Hispanic Black (2.6 percent) non-elderly adults than for Hispanic non-elderly adults (1.0 percent). Poverty status (figure 3) Lower-income non-elderly adults were more likely than those with higher incomes to have any use and frequent use of opioids during the year (figure 3). The percentage of non-elderly adults with at least one opioid prescription fill was highest for those with family incomes below the federal poverty line (13.3 percent), and low-income non-elderly adults were more likely to fill at least one opioid prescription (9.8 percent) than those with middle and high incomes (8.5 percent and 7.4 percent, respectively). Similarly, the rate of frequent use was highest among poor non-elderly adults (5.4 percent), and low-income non-elderly adults were more likely to have frequent opioid use (3.2 percent) than those with middle (2.1 percent) and high incomes (1.4 percent). Insurance coverage (figure 4) This Statistical Brief uses four mutually exclusive categories of insurance: any private insurance, public coverage due to a disability ("public disability-related"), public coverage based on other factors ("public other"), and uninsured. In 2018-2019, non-elderly adults with public disability-related coverage were substantially more likely to fill at least one opioid prescription (30.3 percent) and to fill five or more opioid prescriptions (18.8 percent) compared to those in other insurance categories (figure 4). Among the other three insurance categories, non-elderly adults with public other coverage had the highest rates of any use (10.2 percent) and frequent use (2.7 percent) of opioids, and non-elderly adults with any private insurance were more likely than the uninsured to have at least one opioid fill (8.0 vs. 3.2 percent) and to have five or more opioid fills (1.5 vs. 0.6 percent) during the year. Perceived health status (figure 5) In 2018-2019, the average annual percentages of non-elderly adults who had any use and frequent use of prescription opioids during the year were lowest for those in excellent health (3.9 percent and 0.4 percent), and both measures of opioid use increased in a stepwise fashion across non-elderly adults who were in very good (6.4 percent and 1.0 percent), good (10.1 percent and 2.3 percent), fair (21.5 percent and 8.8 percent), and poor health (36.8 percent and 20.1 percent). Census region (figure 6) In 2018-2019, non-elderly adults in the Northeast and West Census regions were less likely, on average, to fill any opioid prescriptions (6.5 percent and 7.8 percent, respectively) than those in the Midwest and South Census regions (10.6 percent and 9.3 percent, respectively). Similarly, non-elderly adults in the Northeast and West Census regions were less likely to fill five or more opioid prescriptions (1.7 percent and 1.6 percent) than those in the Midwest and South Census regions (2.5 percent and 2.9 percent). MSA status (figure 7) Non-elderly adults living in MSAs were less likely than those living in non-MSAs to fill any outpatient opioid prescriptions (8.2 percent vs. 12.4 percent) and to obtain five or more opioid prescription fills during the year (2.1 percent vs. 3.6 percent). |
||||||||||||||||||
Data SourceThis Statistical Brief uses data from the 2018-2019 MEPS Full Year Consolidated Data Files (HC-209 and HC-216) and non-public versions of the 2018-2019 Prescribed Medicines Files (HC-207A and HC-213A). |
||||||||||||||||||
DefinitionsOpioidsIn this Statistical Brief, we examine outpatient prescription fills of opioids that are commonly used to treat pain. These opioids are identified using generic drug names for narcotic analgesics and narcotic analgesic combinations in the Multum Lexicon database from Cerner Multum, Inc. We identify slightly more opioids commonly used for pain than one would find in the MEPS public use files due to methods used to preserve the confidentiality of sample members. Opioids that are excluded from our analysis include respiratory agents, antitussives and drugs commonly used in medication-assisted treatment. Opioid prescription fills We examine the average annual percentage of non-elderly adults with any outpatient opioid prescription fills during the year ("any use") and the percentage with five or more fills or refills ("frequent use"). Acquisition of five fills or refills represents the 75th percentile of the distribution of prescription fills among all adults (elderly and non-elderly) with any fills during the year. MEPS estimates of opioid use may differ from estimates based on other data sources for several reasons. For example, MEPS and the Substance Abuse and Mental Health Services Administration's National Survey on Drug Use and Health (NSDUH) have substantial differences in methodologies and objectives. The NSDUH any-use estimates comprise both prescribed use and misuse. Misuse includes taking medications for the feeling and in any way a doctor did not prescribe. NSDUH respondents report use in inpatient settings, as well as outpatient. Moreover, NSDUH includes targeted questions with show cards for specific drugs, is self-reported using audio computer-assisted self-interviewing, surveys persons 12 and older, and questions are asked based on a 12-month recall period. In contrast, MEPS includes only prescribed drugs purchased in outpatient settings. Prescription medicines administered in an inpatient setting or in a clinic or physician's office are not included. MEPS data are household-reported, and one respondent reports for the entire household. MEPS uses computer-assisted personal interviewing, and questions are asked using a recall period of 3-6 months. Finally, this Statistical Brief examines opioid use among adults ages 18 to 64. Non-elderly adults This category consists of individuals ages 18 to 64. The age variable used to identify non-elderly adults is based on the sample person's age as of the end of the year. If data were not collected during a round because the sample person was out of scope (e.g., deceased or institutionalized), then age at the time of the previous round was used. Race/ethnicity Classification by race/ethnicity was based on information reported for each family member. First, respondents were asked if the person's main national origin or ancestry was Puerto Rican; Cuban; Mexican, Mexican-American, or Chicano; other Latin American; or other Spanish. All persons whose main national origin or ancestry was reported in one of these Hispanic groups, regardless of racial background, were classified as Hispanic. All other persons were classified according to their reported race. For this analysis, the following classification by race and ethnicity was used: Hispanic, non-Hispanic Black, non-Hispanic White, and non-Hispanic other. The other category includes American Indian, Alaska Native, Asian or Pacific Islander, other race, and multiple races. Poverty status Each sample person was classified according to the total annual income of his or her family. Possible sources of income included annual earnings from wages, salaries, bonuses, tips, and commissions; business and farm gains and losses; unemployment and workers' compensation; interest and dividends; alimony, child support, and other private cash transfers; private pensions, individual retirement account withdrawals, Social Security, and U.S. Department of Veterans Affairs payments; Supplemental Security Income (SSI) and cash welfare payments from public assistance and Temporary Assistance for Needy Families; gains or losses from estates, trusts, partnerships, S corporations, rent, and royalties; and a small amount of "other" income. Poverty status is the ratio of family income to the corresponding federal poverty thresholds, which control for family size and age of the head of family. Categories are defined as follows:
The MEPS respondent was asked to rate the health of each person in the family at the time of the interview according to the following categories: excellent, very good, good, fair, and poor. For persons with missing health status in a round, the response for health status at the previous round was used, if available. A small percentage of persons (less than 1 percent) had a missing response for perceived health status. Census region The Census region variable is based on the location of the household at the end of the year. If missing, the most recent location available is used.
The MSA variable is based on the location of the household at the end of the year and reflects the most recent delineations of MSAs established by Office of Management and Budget. An MSA contains a core urban area of 50,000 or more population. All counties that are not part of an MSA are considered rural. |
||||||||||||||||||
About MEPSThe Medical Expenditure Panel Survey Household Component (MEPS-HC) collects nationally representative data on healthcare use, expenditures, sources of payment, and insurance coverage for the U.S. civilian noninstitutionalized population. The MEPS-HC is cosponsored by the Agency for Healthcare Research and Quality (AHRQ) and the National Center for Health Statistics (NCHS). More information about the MEPS-HC can be found on the MEPS website at https://www.meps.ahrq.gov/. |
||||||||||||||||||
ReferencesFor a detailed description of the MEPS-HC survey design, sample design, and methods used to minimize sources of nonsampling error, see the following publications:Centers for Disease Control and Prevention (CDC). CDC Guideline for Prescribing Opioids for Chronic Pain. U.S. Department of Health and Human Services, CDC. https://www.cdc.gov/drugoverdose/pdf/guidelines_at-a-glance-a.pdf Cohen, J. Design and Methods of the Medical Expenditure Panel Survey Household Component. MEPS Methodology Report No. 1. AHCPR Pub. No. 97-0026. July 1997. Agency for Health Care Policy and Research (AHCPR), Rockville, MD. https://www.meps.ahrq.gov/data_files/publications/mr1/mr1.pdf Cohen, S. Sample Design of the 1996 Medical Expenditure Panel Survey Household Component. MEPS Methodology Report No. 2. AHCPR Pub. No. 97-0027. July 1997. AHCPR, Rockville, MD. https://www.meps.ahrq.gov/data_files/publications/mr2/mr2.pdf Mattson, C. L., Tanz, L. J., Quinn, K., Kariisa, M., Patel, P., and Davis, N. L. (2021). Trends and geographic patterns in drug and synthetic opioid overdose deaths - United States, 2013-2019. Morbidity and Mortality Weekly Report (MMWR), 70(6), 202-207. https://doi.org/10.15585/mmwr.mm7006a4 |
||||||||||||||||||
Suggested CitationMoriya, A. S., and Fang, Z. Any Use and "Frequent Use" of Opioids among Non-Elderly Adults in 2018-2019, by Socioeconomic Characteristics. Statistical Brief #542. March 2022. Agency for Healthcare Research and Quality, Rockville, MD. https://meps.ahrq.gov/data_files/publications/st542/stat542.shtmlAHRQ welcomes questions and comments from readers of this publication who are interested in obtaining more information about access, cost, use, financing, and quality of healthcare in the United States. We also invite you to tell us how you are using this Statistical Brief and other MEPS data and tools and to share suggestions on how MEPS products might be enhanced to further meet your needs. Please email us at MEPSProjectDirector@ahrq.hhs.gov or send a letter to the address below: Joel W. Cohen, PhD, Director Center for Financing, Access and Cost Trends Agency for Healthcare Research and Quality 5600 Fishers Lane, Mailstop 07W41A Rockville, MD 20857 |
||||||||||||||||||
|
||||||||||||||||||
Figure 1. Average annual percentages of non-elderly adults who filled outpatient opioid1 prescriptions in 2018-2019, overall and by sex
Source: Agency for Healthcare Research and Quality, Center for Financing, Access and
Cost Trends, Household Component of the Medical Expenditure Panel Survey,
2018-2019. |
||||||||||||||||||
|
||||||||||||||||||
Figure 2. Average annual percentages of non-elderly adults who filled outpatient opioid1 prescriptions in 2018-2019, by race/ethnicity
Source: Agency for Healthcare Research and Quality, Center for Financing, Access and
Cost Trends, Household Component of the Medical Expenditure Panel Survey, 2018-2019.
|
||||||||||||||||||
|
||||||||||||||||||
Figure 3. Average annual percentages of non-elderly adults who filled outpatient opioid1 prescriptions in 2018-2019, by poverty status
Source: Agency for Healthcare Research and Quality, Center for Financing, Access and
Cost Trends, Household Component of the Medical Expenditure Panel Survey,
2018-2019. |
||||||||||||||||||
|
||||||||||||||||||
Figure 4. Average annual percentages of non-elderly adults who filled outpatient opioid1 prescriptions in 2018-2019, by insurance coverage
Source: Agency for Healthcare Research and Quality, Center for Financing, Access and
Cost Trends, Household Component of the Medical Expenditure Panel Survey,
2018-2019. |
||||||||||||||||||
|
||||||||||||||||||
Figure 5. Average annual percentages of non-elderly adults who filled outpatient opioid1 prescriptions in 2018-2019, by perceived health status
Source: Agency for Healthcare Research and Quality, Center for Financing, Access and
Cost Trends, Household Component of the Medical Expenditure Panel Survey,
2018-2019. |
||||||||||||||||||
|
||||||||||||||||||
Figure 6. Average annual percentages of non-elderly adults who filled outpatient opioid1 prescriptions in 2018-2019, by Census region
Source: Agency for Healthcare Research and Quality, Center for Financing, Access and
Cost Trends, Household Component of the Medical Expenditure Panel Survey,
2018-2019. |
||||||||||||||||||
|
||||||||||||||||||
Figure 7. Average annual percentages of non-elderly adults who filled outpatient opioid1 prescriptions in 2018-2019, by metropolitan statistical area (MSA) status
Source: Agency for Healthcare Research and Quality, Center for Financing, Access and
Cost Trends, Household Component of the Medical Expenditure Panel Survey,
2018-2019. |
| |||||||||||||||||



