Skip to main content
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
STATISTICAL BRIEF #549:
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| July 2023 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Emily Mitchell, PhD, Rebecca Ahrnsbrak, MPS, and Zhengyi Fang, MS
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Highlights
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
IntroductionBy the end of 2020, around 20 million people in the United States had experienced a confirmed case of COVID-19 [1, 2], and certain populations were disproportionately impacted by the disease. Previous studies suggest that some sociodemographic groups, such as racial/ethnic minorities and individuals living in areas with higher poverty levels, experienced higher rates of COVID-19 [3, 4].In this Statistical Brief, we describe COVID-19-related utilization and expenditures for the U.S. civilian noninstitutionalized population in 2020. Note that this population does not include people residing in nursing homes or other institutions, nor does it include active-duty military personnel. We present the percentage of individuals with COVID-19-related ambulatory visits1 and hospital inpatient stays or emergency room (ER) visits, and we highlight differences in COVID-19 treatment and expenditures by demographic groups, including age group, insurance coverage status, income level, race/ethnicity, region, and urbanicity. All differences discussed in the text are statistically significant at the 0.05 level unless otherwise noted. The percentages of people presented in this report are estimates of the treated prevalence for COVID-19, where treatment includes any ambulatory visit, hospital inpatient stay, ER visit, prescribed medicine purchase, or home health visit related to COVID-19. Note that all healthcare utilization in the Medical Expenditure Panel Survey (MEPS) is reported by household respondents, and medical conditions associated with events are not verified by healthcare professionals. The estimates in this Brief represent the treated prevalence of COVID-19, which differs from the true prevalence of COVID-19. Estimates of true prevalence attempt to capture the number of people with COVID-19, regardless of whether they received medical care related to the disease. Treated prevalence is a subset of true prevalence because it represents people who had COVID-19 and had a medical event related to COVID-19. Estimates of both treated prevalence from MEPS and overall prevalence estimates from other sources may underestimate the true disease prevalence in 2020 due to limited availability of COVID-19 testing early in the pandemic and lack of reporting of at-home test results to public health authorities. In addition, as noted above, MEPS utilization estimates are reported by household respondents, and as such can be susceptible to recall bias and reporting error. The onset of the COVID-19 pandemic created additional concerns about reporting accuracy, due to impacts on MEPS field operations and response mode and lower response rates. Most MEPS interviews switched from in-person to phone and video modes during the early stages of the pandemic. However, recent analyses indicate that these changes did not adversely affect the quality of reporting healthcare use in MEPS [5]. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
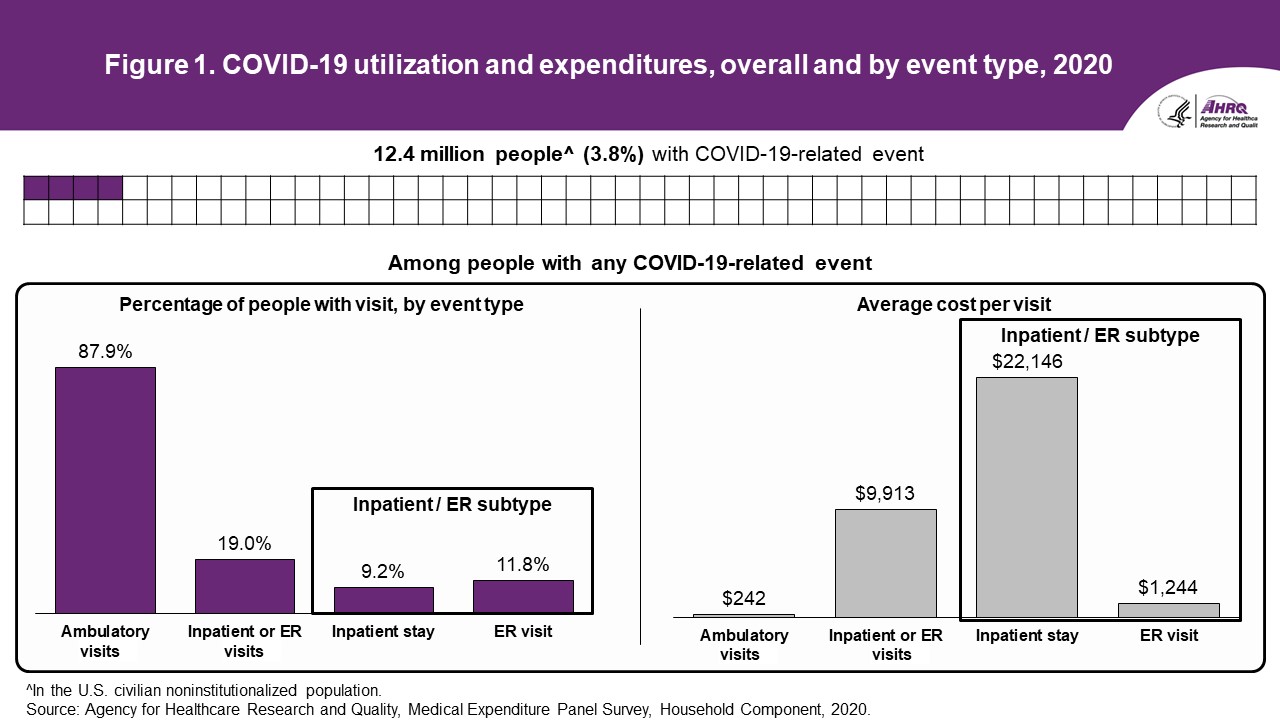
FindingsOverall (figure 1 and table 1)According to data from the 2020 MEPS, over 12.4 million people (3.8 percent) in the U.S. civilian noninstitutionalized population received treatment for COVID-19 during 2020. Total expenditures for COVID-19-related treatment were around $33 billion, with treatment averaging around $2,678 per person with care for COVID-19.Among people with any COVID-19 treatment, a majority (87.9 percent) had at least one ambulatory visit. The average cost for COVID-19-related ambulatory visits was $242. While fewer people had an inpatient hospital stay or ER visit (19.0 percent), these events were much more expensive, averaging $9,913 per event. Looking at these events by subtype, average costs per event were around $22,146 for inpatient stays, and $1,244 for ER visits. Table 1. Healthcare use and expenditures among people with any COVID-19 treatment, by event type, 2020
* An ambulatory visit is an office-based medical visit or hospital outpatient department visit Note that while overall treated prevalence for COVID-19 includes people with home health visits and prescribed medicine purchases, we do not report estimates for these event types for the following reasons:
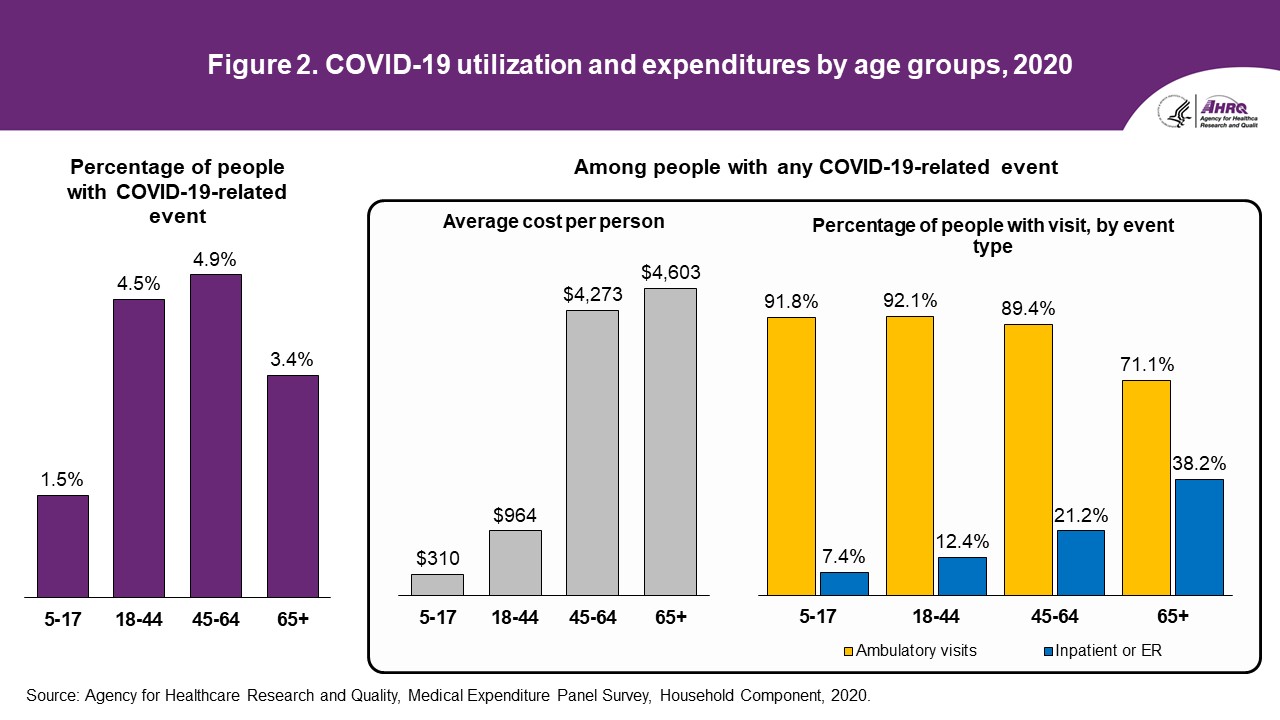
Age groups (figure 2 and tables 2a,b)Nearly 5 percent of adults between the ages of 45 and 64 and 4.5 percent of adults ages 18-44 had a medical visit or prescribed medicine purchase for COVID-19 in 2020. These age groups were more likely to have a COVID-19-related event than children ages 5-17.2Among people with any COVID-19 treatment, average per-person costs for COVID-19-related events were over $4,000 for people older than 45, while average costs for children ages 5-17 and younger adults (ages 18-44) were under $1,000 per person. This difference is partially attributable to the fact that older adults were more likely to have a hospital inpatient stay or emergency room visit (38.2 percent of adults ages 65+ vs. 12.4 percent of adults ages 18-44), which tend to be more expensive than ambulatory visits. Table 2a. Treated prevalence for COVID-19, by age group, 2020
Table 2b. Healthcare use and expenditures among people with any COVID-19 treatment, by age group, 2020
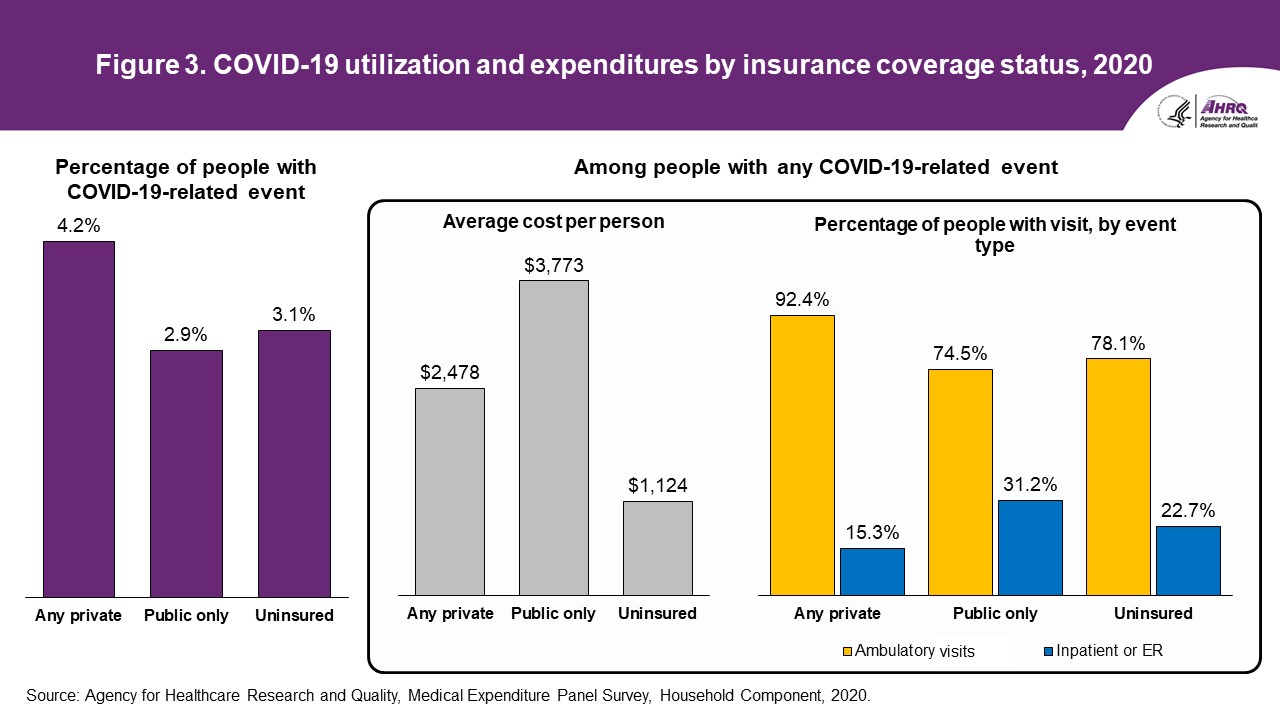
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. Insurance coverage (figure 3 and tables 3a,b)People with any private insurance in 2020 were more likely to receive treatment for COVID-19 than people with only public insurance, and this was true for all ages (4.2 percent vs. 2.9 percent) as well as those under age 65 (4.3 percent vs. 2.9 percent). Similarly, people ages 65 and over with Medicare and private insurance were more likely to have treatment for COVID-19 than people with Medicare and other public insurance (3.8 percent vs. 1.9 percent).Among people with any treatment for COVID-19, those with private insurance were more likely to have an ambulatory visit for COVID-19 than people with only public insurance, for all ages (92.4 percent vs. 74.5 percent) as well as those under 65 (94.3 percent vs. 80.3 percent). Conversely, people with only public insurance were more likely to have an inpatient stay or ER visit than those with private insurance, for all ages (31.2 percent vs. 15.3 percent) as well as those under age 65 (25.7 percent vs. 12.7 percent). As noted previously, persons over age 65 with COVID-19 treatment were more likely to have an inpatient stay or ER visit than persons under age 65. However, among older people (ages 65+) there were no significant differences in the percentages of people with an inpatient stay or ER visit by insurance coverage. Although the percentage of uninsured people with inpatient or ER visits was not statistically different from people with only public insurance, average per-person expenditures for COVID-19-related treatment were lower for uninsured people than for those with only public insurance, as well as for those with any private coverage. Table 3a. Treated prevalence for COVID-19, by insurance coverage status and age, 2020
* Persons age 65+ who reported no Medicare are excluded from the insurance coverage by age categories due to small sample size. Table 3b. Healthcare use and expenditures among people with any COVID-19 treatment, by insurance coverage status and age, 2020
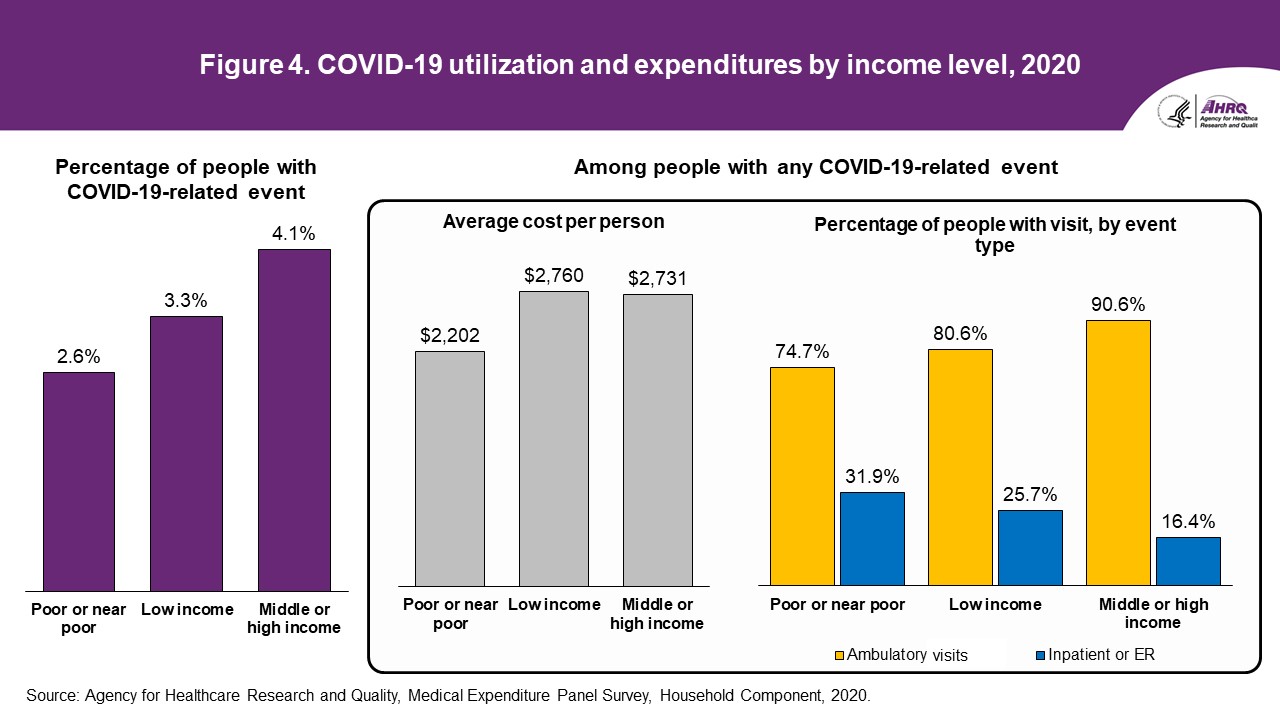
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. Income (figure 4 and tables 4a,b)People with middle or high income were more likely to have COVID-19-related treatment in 2020 than people with poor or near-poor income levels (4.1 percent vs. 2.6 percent). Among people with any COVID-19 treatment, those with higher income were also more likely to have an ambulatory visit than people with lower income (90.6 percent vs. 74.7 percent) and less likely to have an inpatient stay or ER visit than people with lower income (16.4 percent vs. 31.9 percent). Despite these differences in event-specific utilization, there were no statistically significant differences in average per-person expenditures across income levels.Table 4a. Treated prevalence for COVID-19, by income level, 2020
Table 4b. Healthcare use and expenditures among people with any COVID-19 treatment, by income level, 2020
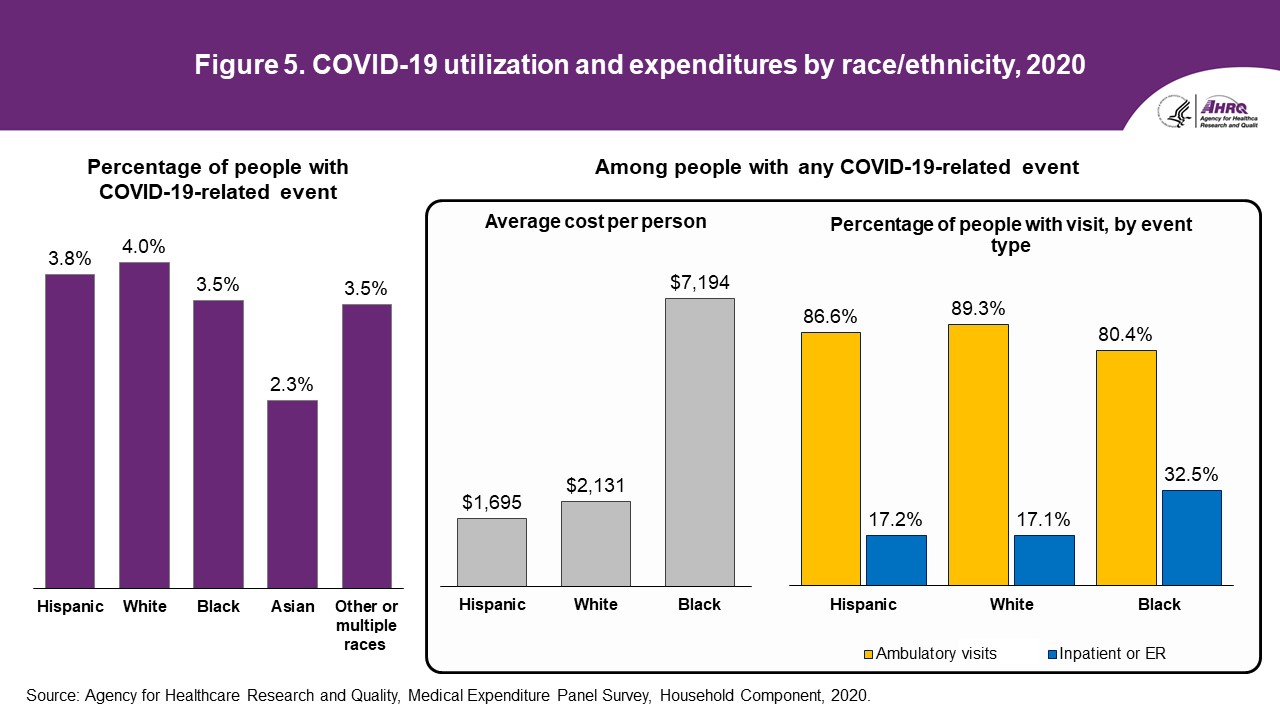
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. Race/ethnicity (figure 5 and tables 5a,b)Asian people were less likely to have treatment for COVID-19 in 2020 compared to White non-Hispanic people (2.3 percent vs. 4.0 percent). Among people with any treatment for COVID-19, Black non-Hispanic people were more likely to have an inpatient stay or ER visit for COVID-19 (32.5 percent) than White non-Hispanic people (17.1 percent). Average per-person expenditures for Black non-Hispanics were around $7,194, compared to average per-person expenditures of around $2,131 for White non-Hispanics. Despite this large apparent discrepancy in expenditures, this difference was only statistically significant at the 0.1 significance level, due to the higher level of uncertainty around the point estimates for average expenditures.Table 5a. Treated prevalence for COVID-19, by race/ethnicity, 2020
Table 5b. Healthcare use and expenditures among people with any COVID-19 treatment, by race/ethnicity, 2020
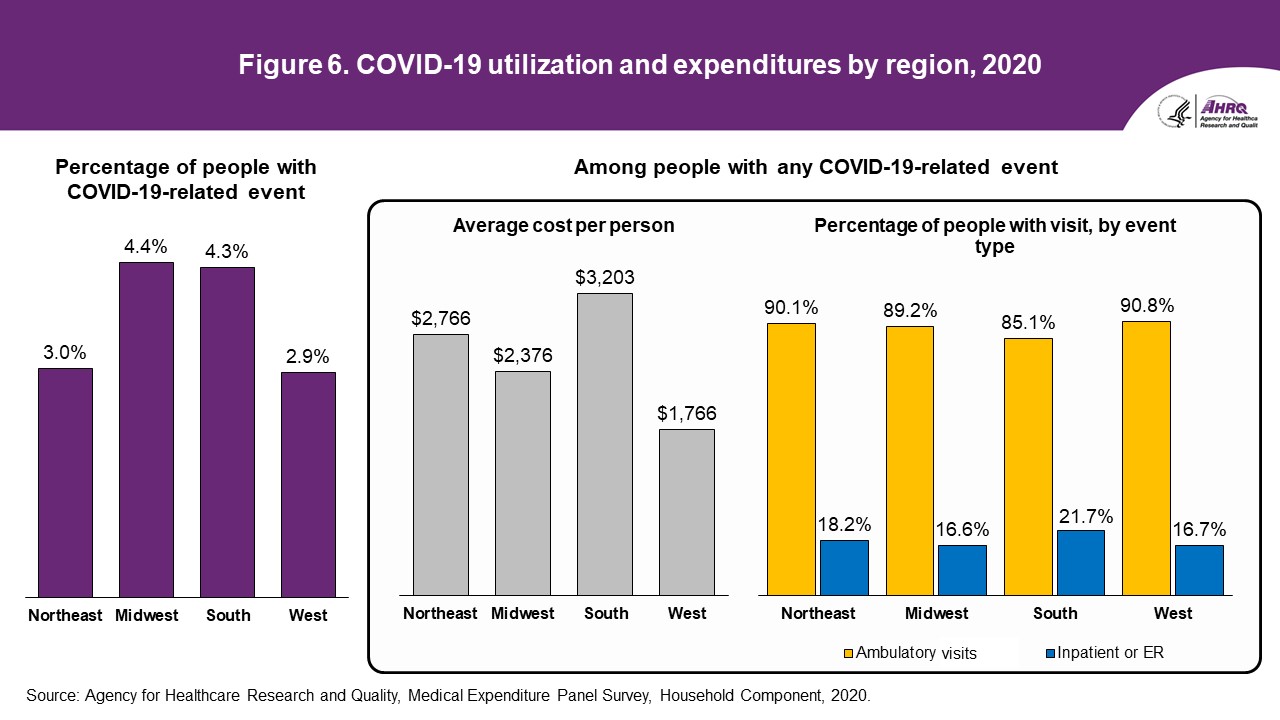
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. Region (figure 6 and tables 6a,b)Over 4 percent of people living in the Midwest or South received treatment for COVID-19 in 2020, compared with around 3 percent of people living in the Northeast or West. Other differences between average per-person expenditures as well as percentages of people with ambulatory or hospital or ER visits were not statistically different across regions.Table 6a. Treated prevalence for COVID-19, by region, 2020
Table 6b. Healthcare use and expenditures among people with any COVID-19 treatment, by region, 2020
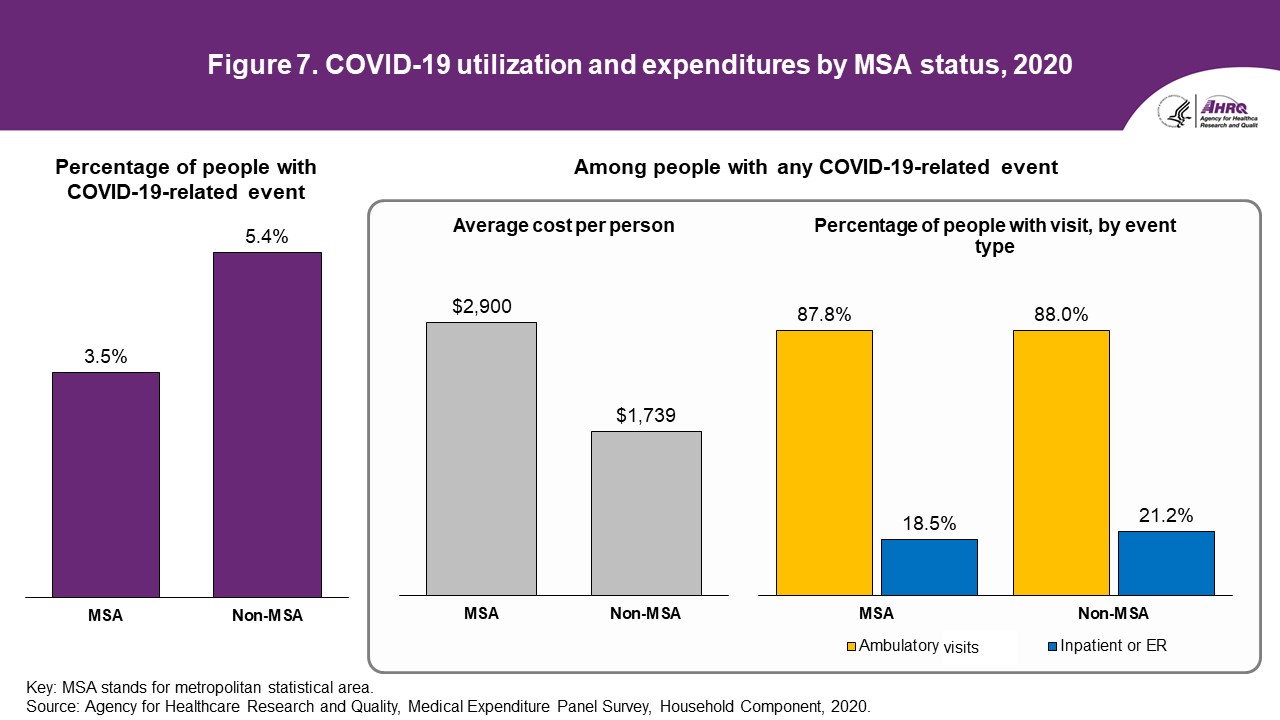
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. Urbanicity (figure 7 and tables 7a,b)Around 5.4 percent of people living in more rural areas (defined as living outside of a metropolitan statistical area [MSA]) received treatment for COVID-19, which was higher than the percentage of people living in more urban areas (3.5 percent).Among people with any COVID-19 treatment, those living in more urban areas had higher average per-person expenditures for COVID-19 than those living in more rural areas ($2,900 for MSA vs. $1,739 for non-MSA), although this difference was only statistically significant at the 0.1 significance level. Other differences between average per-person expenditures as well as percentages of people with ambulatory or hospital or ER visits were not statistically different across urbanicity. Table 7a. Treated prevalence for COVID-19, by urbanicity, 2020
Table 7b. Healthcare use and expenditures among people with any COVID-19 treatment, by urbanicity, 2020
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Data SourceThe estimates reported in this Brief are based on data from the following MEPS data files:
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
DefinitionsAgeAge is defined as age at the end of the year 2020 (or on last date of MEPS eligibility if person was out of scope at the end of the year). COVID-19A person in the MEPS sample is defined as having treatment for COVID-19 if the household respondent reports one or more healthcare events (i.e., office-based, hospital outpatient or ER visits, hospital inpatient stays, prescribed medicine purchases, or home healthcare) where the respondent reported that COVID-19 led to or was discovered during the event. COVID-19 conditions can be identified on the MEPS Medical Conditions Public Use Files with an International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) code starting with "U07" (ICD10CDX = "U07"). Event type
ExpendituresTotal expenditures are defined as the sum of payments from all sources to hospitals, physicians, other healthcare providers, and pharmacies for services reported by respondents in the Medical Expenditure Panel Survey Household Component (MEPS-HC). IncomeThree income groups are defined based on the percentage of the poverty line for total family income, adjusted for family size and composition. We use three categories:
Insurance coverage
Insurance coverage by age
Race/ethnicityMEPS respondents were asked if each family member was Hispanic or Latino and about each member's race. Based on this information, categories of race and Hispanic origin were constructed as follows:
RegionEach sample person was classified as living in one of the following four regions as defined by the U.S. Bureau of the Census:
UrbanicityIndividuals were identified as residing either inside or outside an MSA as designated by the U.S. Office of Management and Budget. An MSA is a large population nucleus combined with adjacent communities that have a high degree of economic and social integration within the nucleus. Each MSA has one or more central counties containing the area's main population concentration. In New England, metropolitan areas consist of cities and towns rather than whole counties. Regions of residence are in accordance with the U.S. Bureau of the Census definition. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
About MEPSThe Medical Expenditure Panel Survey Household Component (MEPS-HC) collects nationally representative data on healthcare use, expenditures, sources of payment, and insurance coverage for the U.S. civilian noninstitutionalized population. The MEPS-HC is cosponsored by the Agency for Healthcare Research and Quality (AHRQ) and the National Center for Health Statistics (NCHS). More information about the MEPS-HC can be found on the MEPS website at https://www.meps.ahrq.gov/. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
ReferencesFor a detailed description of the MEPS-HC survey design, sample design, and methods used to minimize sources of nonsampling error, see the following publications:
The following methodology reports contain information on the survey and sample designs for the MEPS-HC and MEPS-Medical Provider Component (MEPS-MPC). Data collected in these two components are jointly used to derive MEPS healthcare expenditure data. Cohen, J. Design and Methods of the Medical Expenditure Panel Survey Household Component. MEPS Methodology Report #1. AHCPR Pub. No. 97-0026. July 1997. Agency for Health Care Policy and Research (AHCPR), Rockville, MD. http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr1/mr1.pdf Ezzati-Rice, T. M., Rohde, F., and Greenblatt, J. Sample Design of the Medical Expenditure Panel Survey Household Component, 1998-2007. Methodology Report #22. March 2008. Agency for Healthcare Research and Quality, Rockville, MD. http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr22/mr22.pdf Machlin, S. R., Chowdhury, S. R., Ezzati-Rice, T., DiGaetano, R., Goksel, H., Wun, L.-M., Yu, W., and Kashihara, D. Estimation Procedures for the Medical Expenditure Panel Survey Household Component. Methodology Report #24. September 2010. Agency for Healthcare Research and Quality, Rockville, MD. https://www.meps.ahrq.gov/data_files/publications/mr24/mr24.shtml Stagnitti, M. N., Beauregard, K., and Solis, A. Design, Methods, and Field Results of the Medical Expenditure Panel Survey Medical Provider Component (MEPS MPC)—2006 Calendar Year Data. Methodology Report #23. November 2008. Agency for Healthcare Research and Quality, Rockville, MD. http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr23/mr23.pdf |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Suggested CitationMitchell, E. M., Ahrnsbrak, R. D., & Fang, Z. Healthcare Use and Expenditures for COVID-19, U.S. Civilian Noninstitutionalized Population, 2020. Statistical Brief #549. July 2023. Agency for Healthcare Research and Quality, Rockville, MD. https://meps.ahrq.gov/data_files/publications/st549/stat549.shtmlAHRQ welcomes questions and comments from readers of this publication who are interested in obtaining more information about access, cost, use, financing, and quality of healthcare in the United States. We also invite you to tell us how you are using this Statistical Brief and other MEPS data and tools and to share suggestions on how MEPS products might be enhanced to further meet your needs. Please email us at MEPSProjectDirector@ahrq.hhs.gov or send a letter to the address below: Joel W. Cohen, PhD, Director Center for Financing, Access and Cost Trends Agency for Healthcare Research and Quality 5600 Fishers Lane, Mailstop 07W41A Rockville, MD 20857 |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 1. Healthcare use and expenditures among people with any COVID-19 treatment^, by event type, 2020
^ Over 12.4 million people (3.8 percent) in the U.S. civilian noninstitutionalized population received treatment for COVID-19 during 2020. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 2a. Treated prevalence for COVID-19, by age group, 2020
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2020. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 2b. Healthcare use and expenditures among people with any COVID-19 treatment, by age group, 2020
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 3a. Treated prevalence for COVID-19, by insurance coverage status, 2020
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2020. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 3b. Healthcare use and expenditures among people with any COVID-19 treatment, by insurance coverage status, 2020
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 4a. Treated prevalence for COVID-19, by income level, 2020
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2020. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 4b. Healthcare use and expenditures among people with any COVID-19 treatment, by income level, 2020
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 5a. Treated prevalence for COVID-19, by race/ethnicity, 2020
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2020. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 5b. Healthcare use and expenditures among people with any COVID-19 treatment, by race/ethnicity, 2020
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 6a. Treated prevalence for COVID-19, by region, 2020
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2020. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 6b. Healthcare use and expenditures among people with any COVID-19 treatment, by region, 2020
* Relative standard error is greater than 30%, indicating higher uncertainty around the accuracy of this estimate. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 7a. Treated prevalence for COVID-19, by urbanicity, 2020
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2020. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Figure 7b. Healthcare use and expenditures among people with any COVID-19 treatment, by urbanicity, 2020
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2020. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
1 In this Statistical Brief, ambulatory visits include office-based medical visits or hospital
outpatient visits. Both in-person and telehealth visits are included. 2 The number of children under age 5 with COVID-19-related treatment was too small to present reliable estimates for this age group. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||



